Cell Rep:NIH研究表明,高活性免疫与衰老性脑疾病有关
2019-01-30 佚名 生物通
NIH/国家神经疾病与中风研究所的一项果蝇研究指出,人体的免疫系统可能在大脑老化损伤中起关键作用。研究结果基于改变Cdk5基因活性后,大脑老化过程加速,导致果蝇更早死亡,并在晚年时期患有飞行或行走障碍,以及更多的神经变性脑损伤迹象。
脑细胞排污系统崩溃,会引发更具破坏性的免疫反应。
NIH/国家神经疾病与中风研究所的一项果蝇研究指出,人体的免疫系统可能在大脑老化损伤中起关键作用。研究结果基于改变Cdk5基因活性后,大脑老化过程加速,导致果蝇更早死亡,并在晚年时期患有飞行或行走障碍,以及更多的神经变性脑损伤迹象。
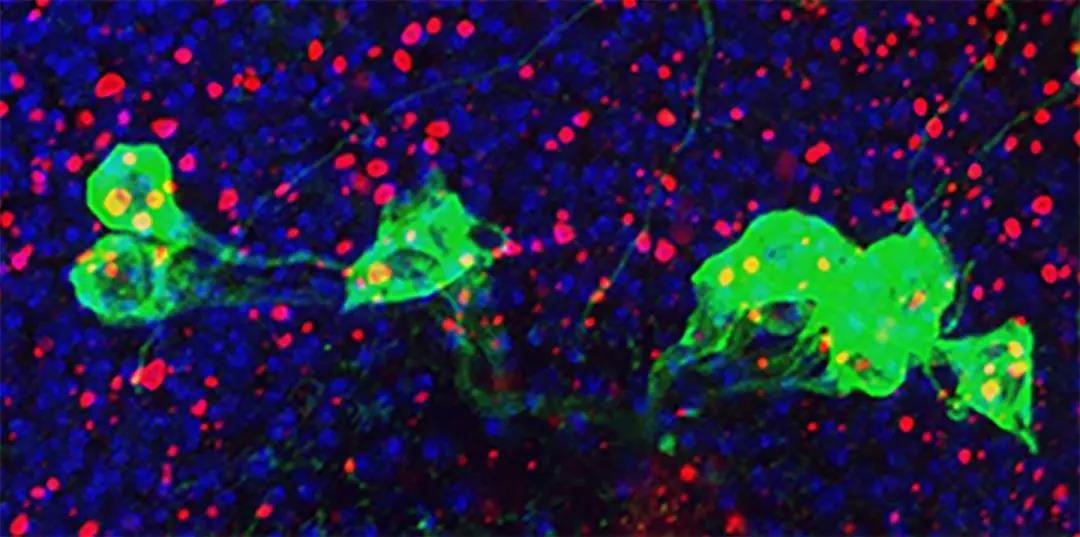
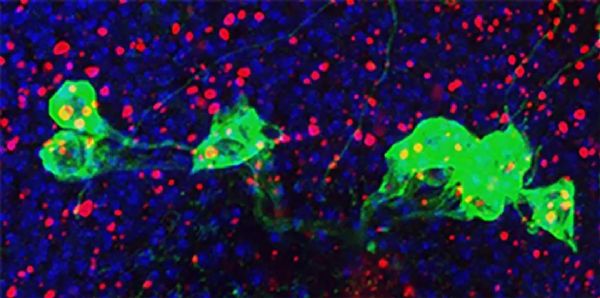
临床前研究表明,Cdk5是对大脑早期发育很重要的基因,可能与神经退行性疾病有关。新研究发表在Cell Reports,文中,作者认为改变Cdk会导致多巴胺释放神经元死亡,对老年果蝇大脑影响尤其严重。通常情况,帕金森症损害人类相同类型细胞。果蝇研究进一步指出,神经元丢失是因为Cdk减缓了细胞自噬,或者说是细胞的排污处理系统,一种受控制的将受损细胞从体内清除的方式,从而触发免疫系统攻击自身神经元。
免疫系统攻击是一个比自噬更混乱更扩散的过程。通过基因修复排污系统或阻断免疫系统反应,就可以阻止Cdk变化引起的多巴胺神经元减少。
作者得出结论,这种连锁反应的根本是自噬紊乱引发了更广泛的破坏性免疫反应,这些反应可能存在于几种人类神经退行性疾病中,研究人员希望从中寻找新的治疗目标和策略。
原始出处:Shukla AK1, Spurrier J2, Kuzina I1, Giniger E3. Hyperactive Innate Immunity Causes Degeneration of Dopamine Neurons upon Altering Activity of Cdk5. Cell Rep. 2019 Jan 2;26(1):131-144.e4.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#Cell#
33
#脑疾病#
38
#CEL#
36
#NIH#
35
向科研人员致敬!!!
66