一文读懂!神经源性膀胱的影像学表现
2022-02-11 医学影像服务中心 医学影像服务中心
中枢或周围神经损害所引起的下尿路贮尿、排尿功能障碍称作神经源性尿道机能障碍,习惯上简称为神经源性膀胱。
中枢或周围神经损害所引起的下尿路贮尿、排尿功能障碍称作神经源性尿道机能障碍,习惯上简称为神经源性膀胱。
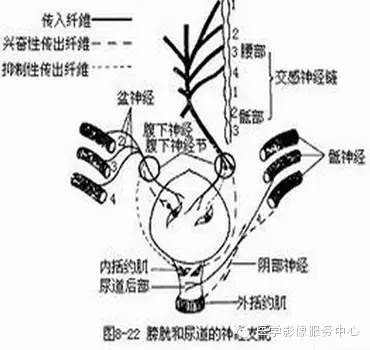
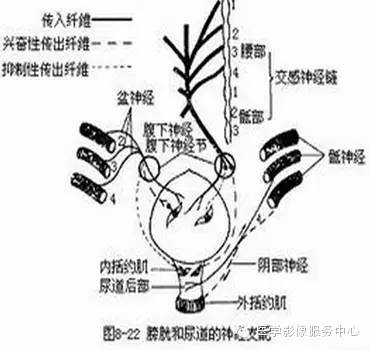
膀胱的存储和排空功能需要膀胱逼尿肌、扩约肌和盆底肌肉之间复杂的神经-肌肉协调和配合来完成。
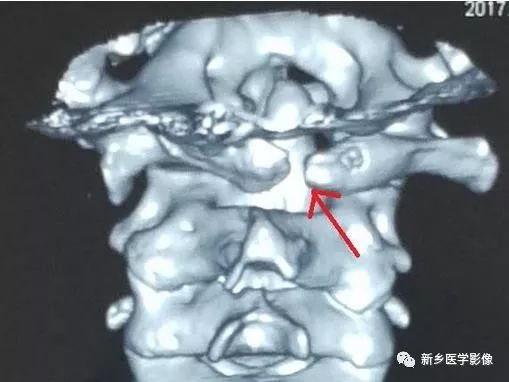
支配会阴三角区肌肉的脊髓排尿中枢位于T11-L2 脊髓节段,支配逼尿肌者位于S2-S4节段,通过锥体束进行协调和抑制。
图像:
中枢或周围神经损害所引起的下尿路贮尿、排尿功能障碍称作神经源性尿道机能障碍,习惯上简称为神经源性膀胱。
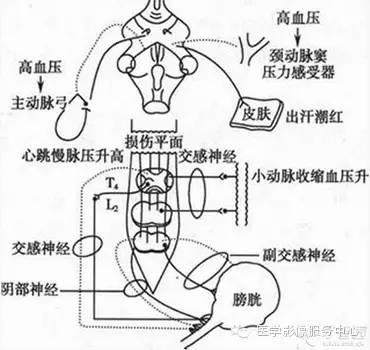
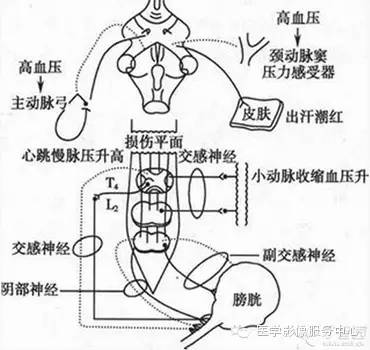
主要病因为中枢神经系统病变,导致排尿反射过强,膀胱频发性不随意强烈收缩,括约肌功能紊乱,导致逼尿肌和括约肌增生与肥厚。
神经系统病变常见于脑肿瘤、脑血管意外、脑脓肿、多发性硬化、Parkinson病、脊髓横断、脊髓压迫等。
临床表现:频发性小便失禁或尿残留。
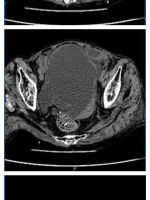
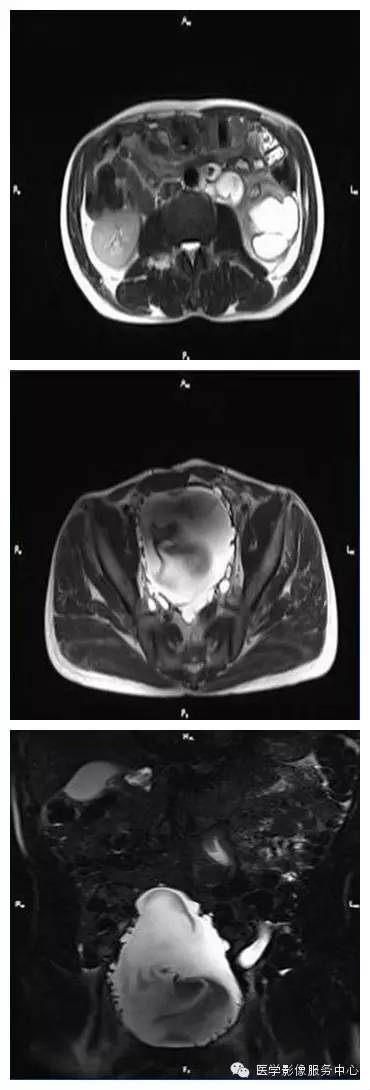
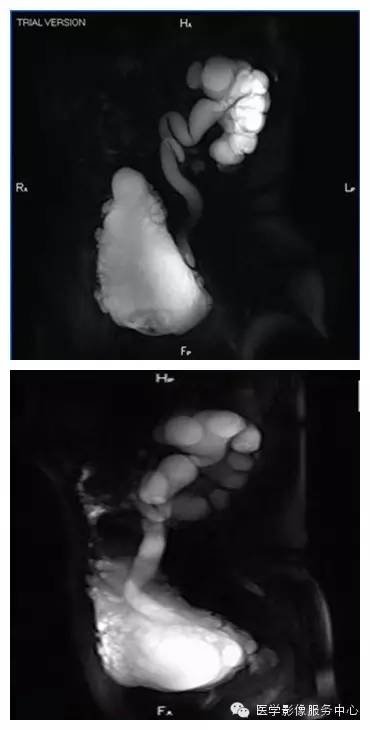
图像:
膀胱造影:由于长期的内压增高,膀胱肌肉增粗肥大形成大小不等的肌肉束。造影可显示膀胱壁边缘高低不平,呈很多波浪状向内凹陷的小梁样结构,即膀胱成梁征象;小梁之间可见多发的小憩室影,憩室大小不一,散在分布;因肌肉小梁增生、肥厚、膀胱颈部明显狭窄。
膀胱增大,呈宝塔样或圣诞树样;有不同程度输尿管逆流,输尿管增宽,肾盂扩张积水,多呈双侧性;可合并膀胱结石等。


CT:平扫时可见膀胱壁增厚,整个膀胱凹凸不平,有部分壁呈双层状或憩室状,两侧输尿管明显扩张,严重者可见两侧肾积水。

MR:可显示膀胱壁增厚,膀胱增大、双肾盂积水、输尿管扩张等。
鉴别诊断:需要与尿路梗阻性疾病,如前列腺肥大、尿道狭窄等造成的尿潴留相鉴别。可通过B超检查和尿道造影,结合临床病史不难鉴别。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#神经源#
57
#神经源性#
0
#神经源性膀胱#
56
好文章,学习到了,谢谢。
0