Int J Med Sci:褪黑素通过AMPK激活减轻氧化应激抑制人骨髓间充质干细胞的成骨作用
2018-07-20 MedSci MedSci原创
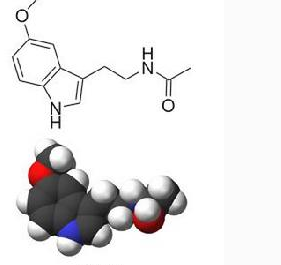
氧化应激通过增加骨吸收或减少骨形成在衰老相关的骨质疏松症的发病机理中起重要作用。褪黑激素可通过抗氧化、抗炎和保骨作用发挥有益作用,或可预防氧化应激抑制的骨生成。然而,褪黑激素拯救氧化应激抑制人间充质干细胞(MSCs)成骨的特定机制尚未完全阐明。因此,本研究探究了褪黑激素对AMPK的激活是否调节人MSCs中氧化应激和成骨分化之间的拮抗串扰。 结果显示,褪黑素通过激活AMPK和上调FOXO3a和
氧化应激通过增加骨吸收或减少骨形成在衰老相关的骨质疏松症的发病机理中起重要作用。褪黑激素可通过抗氧化、抗炎和保骨作用发挥有益作用,或可预防氧化应激抑制的骨生成。然而,褪黑激素拯救氧化应激抑制人间充质干细胞(MSCs)成骨的特定机制尚未完全阐明。因此,本研究探究了褪黑激素对AMPK的激活是否调节人MSCs中氧化应激和成骨分化之间的拮抗串扰。
结果显示,褪黑素通过激活AMPK和上调FOXO3a和RUNX2显著增强人MSCs的成骨分化,FOXO3a和RUNX2是参与联系氧化应激和成骨表型的主要转录因子。通过褪黑激素治疗氧化应激,钙沉积结果显示成骨分化显著增加。此外,褪黑素处理活化AMPK的和氧化应激抑制的FOXO3a和RUNX2的表达。
总体而言,这些结果表明褪黑激素增强人MSCs的成骨分化,并通过人MSCs中的AMPK活化恢复氧化应激抑制的骨生成,表明褪黑激素激活AMPK或可用于治疗代谢性骨病,如骨质疏松症。
原始出处:
Lee S, Le NH, Kang D. Melatonin alleviates oxidative stress-inhibited osteogenesis of human bone marrow-derived mesenchymal stem cells through AMPK activation. Int J Med Sci. 2018 Jun 23;15(10):1083-1091. doi: 10.7150/ijms.26314. eCollection 2018.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#间充质干细#
39
#骨髓间充质干细胞#
39
学了
85
#成骨#
34
#应激#
42
#Med#
29
学习了谢谢
66
阅
66
褪黑素抑制人骨髓间充质干细胞的成骨作用。
63
我就
77