JAHA:hsTnI水平与冠状动脉病变的严重程度、进展和长期预后!
2018-02-22 xing.T MedSci原创
由此可见,高hsTnI水平与冠状动脉粥样硬化的潜在负担、CAD进展更快速以及高风险的全因死亡和心血管事件相关。更积极的旨在降低hsTnI水平的治疗是否可以调节疾病的进展,需要进一步调查。
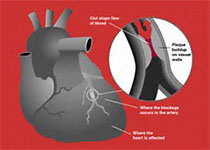
高敏肌钙蛋白I(hsTnI)水平与冠状动脉疾病(CAD)严重程度和进展之间的关联仍不清楚。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员旨在明确hsTnI是否与CAD的严重程度和进展相关,并且hsTnI水平对心血管结局事件的预测价值是否独立于CAD严重程度。
该研究纳入了3087名(63±12岁,64%为男性)接受心导管检查的无急性心肌梗死证据的患者,通过狭窄≥50%的主要冠状动脉的数量和Gensini评分来计算CAD严重程度。研究人员对717例招募前超过3个月期间接受超过2次的冠状动脉造影的亚组评估CAD进展。研究人员随访了患者的所有原因死亡和心血管事件。
在总人群中,11%的受试者造影正常,23%的受试者为阻塞性CAD,20%的受试者为一支血管CAD,20%的受试者为二支血管CAD,26%的受试者为三支血管CAD。在调整了年龄、性别、种族、体重指数、吸烟、高血压、糖尿病史和肾功能后,hsTnI水平与冠心病Gensini评分评估的CAD严重程度(Log2ß=0.31;95%可信区间为0.18-0.44;P<0.001)和CAD进展(Log2ß=0.36;95%可信区间为0.14-0.58;P=0.001)独立相关。hsTnI水平也是心血管事件死亡、死亡、心肌梗死、血运重建和心脏住院的重要的预测因子,独立于上述变量和CAD严重程度。
由此可见,高hsTnI水平与冠状动脉粥样硬化的潜在负担、CAD进展更快速以及高风险的全因死亡和心血管事件相关。更积极的旨在降低hsTnI水平的治疗是否可以调节疾病的进展,需要进一步调查。
原始出处:
Ayman Samman Tahhan,et al. High‐Sensitivity Troponin I Levels and Coronary Artery Disease Severity, Progression, and Long‐Term Outcomes.JAHA.2018. https://doi.org/10.1161/JAHA.117.007914
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#冠状动脉病变#
38
#长期预后#
31
学习了感谢分享
71
学习了感谢分享
75
#AHA#
35
学习
64