JAHA:支架内血栓形成后的长期预后和死亡的临床预测因素
2022-04-06 MedSci原创 MedSci原创
ST后10年累积死亡率达到33.8%。因此,对于ST患者,尤其是血液透析患者、左主干和左冠状动脉病变患者以及肌酸激酶峰值患者,必须进行密切的随访。
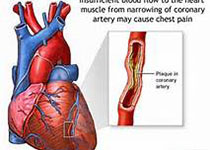
药物洗脱支架(DESs)通常用于冠状动脉疾病的治疗。尽管与裸金属支架相比,DESs显著降低了再狭窄的发生率,但与支架血栓形成(ST)相关的问题有所增加,特别是晚期支架血栓形成和非常晚期的支架血栓形成,分别发生在支架植入后1个月和1年。支架植入术后又因血栓的突然发作而引起急性心肌梗死和猝死。支架血栓形成(ST)仍然是一个重要的医学问题。特别是,ST发生后的长期死亡率和临床预测因素尚未阐明。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,这项多中心、回顾性、观察性研究从2008年1月到2017年12月期间共纳入了187例确定的ST病例,并对其长期临床结局进行了调查。该研究的主要终点指标是ST发生后的累积死亡率。此外,研究人员还评估了死亡率的独立预测因子。

在导致ST的支架类型中,裸金属支架、第一代药物洗脱支架、第二代药物洗脱支架和第三代药物洗脱支架分别占31.0%、19.3%、36.9%和6.4%。从支架植入到ST的中位持续时间为680.5天(四分位数范围为33.8-2450.5天)。1、2、3、5、10年累积死亡率分别为14.6%、17.4%、21.2%、24.4%和33.8%。不同支架类型的累积死亡率无显著差异,晚期ST段的死亡率高于早期ST段和极晚期ST段;但多元分析后,无统计学意义。

死亡率的独立预测因素是血液透析(风险比[HR]为7.80;95%置信区间为3.07-19.81;P<0.001),左主干的罪犯病变(HR为8.14;95%置信区间为1.71-38.75;P=0.008)、左冠状动脉罪犯病变(HR为2.77;95%置信区间为1.10-6.96;P=0.030)、肌酸激酶峰值(HR为1.017;95%置信区间为1.011-11.022;P<0.001)。
由此可见,ST后10年累积死亡率达到33.8%。因此,对于ST患者,尤其是血液透析患者、左主干和左冠状动脉病变患者以及肌酸激酶峰值患者,必须进行密切的随访。
原始出处:
Takayuki Ishihara,et al.Long‐Term Outcomes and Clinical Predictors of Mortality Following Occurrence of Stent Thrombosis.JAHA.2022.https://www.ahajournals.org/doi/10.1161/JAHA.121.023276.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#支架内血栓#
32
#长期预后#
29
#预测因素#
51
#AHA#
37