JACC:心脏术前I型胶原和III型胶原合成相关的血清肽浓度升高增加术后房颤发生的风险
2012-11-26 JACC JACC
房颤是心脏术后常见的并发症,据统计其发生率高达30%,且术后房颤的发生是增加术后死亡率的独立预测因子。目前认为心脏术后房颤多源于左心房,且术前的心房纤维化在其中起主要作用。左心室肥厚及舒张功能减退导致左心房内张力增大,诱发细胞外基质的重构,因此我们认为心房纤维化的血清学及组织学标志物升高可预测心脏术后房颤的发生。 左房纤维化主要是指I型胶原和III型胶原合成增加,它们由成纤维细胞
房颤是心脏术后常见的并发症,据统计其发生率高达30%,且术后房颤的发生是增加术后死亡率的独立预测因子。目前认为心脏术后房颤多源于左心房,且术前的心房纤维化在其中起主要作用。左心室肥厚及舒张功能减退导致左心房内张力增大,诱发细胞外基质的重构,因此我们认为心房纤维化的血清学及组织学标志物升高可预测心脏术后房颤的发生。
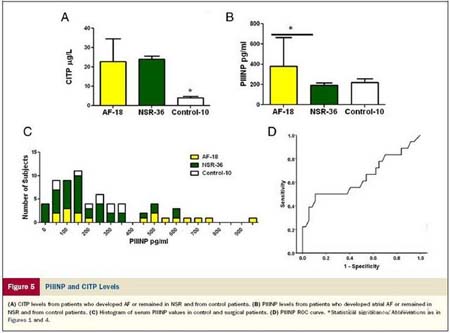
左房纤维化主要是指I型胶原和III型胶原合成增加,它们由成纤维细胞和肌成纤维细胞合成,受TGF-β和Ang-II调控。前I型胶原羧基末端肽(PICP)和前III型胶原氨基末端肽(PIIINP)分别是I型胶原和III型胶原合成过程中的产物,它们的浓度可反应I型胶原和III型胶原合成的速度。然而目前关于PICP和PIIINP是否能预测心脏术后房颤的发生还不明确。据此Swartz MF等进行了一项临床研究,旨在探讨PICP及PIIINP与心房纤维化及心脏术后房颤发生的关系。
研究共入院54例既往无房颤发作的接受心脏手术患者,所有患者术前进行抽血检查,术中进行左心房及右心房活检。应用天狼星红染色评估心房纤维化程度,应用RT-PCR技术测定参与I型胶原及III型胶原合成过程中的相关信使蛋白,采用酶联免疫吸附法测定PICP和PIIINP浓度。
结果显示共用18例患者术后发生了房颤,其余36例始终维持窦律。与维持窦律者比较,发生房颤的患者心房纤维比例显著增高(6.19±2.9%比2.03±1.9%,p=0.03),在发生房颤的患者,TGF-β和Ang-II的表达较维持窦律者升高了1.5-2.0倍。血清PICP及PIIINP浓度显著高于维持窦律者。血清PICP与心房纤维化之间存在明显的线性关系,PICP浓度是心脏术后房颤发生的独立预测因子。
通过该项研究,作者得出以下结论:血清PICP及PIIINP浓度升高与心房纤维化呈密切相关,它们可作为术前无房颤的患者心脏术后发生房颤的独立预测因子。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#血清肽#
27
#JACC#
27
#III#
30
#术后房颤#
27
#ACC#
35
#浓度#
36