BMC Cancer:仑伐替尼联合PD-1抑制剂治疗晚期肝细胞癌的真实世界疗效
2022-03-24 yd2015 网络
研究表明,仑伐替尼联合PD-1抑制剂可为晚期HCC伴有Vp4患者带来生存获益。
近期,浙江大学附属第一医院和中山大学肿瘤防治中心的团队在BMC Cancer杂志上发表了一项研究成果,主要是评估仑伐替尼联合PD-1抑制剂治疗晚期肝细胞癌患者的疗效,尤其是肿瘤占据肝脏体积≧50%(TO ≥50%)或Vp4侵犯。
研究纳入84例患者,中位年龄为53岁。大多数为男性(n=69)。大多数患者感染了乙型肝炎病毒。85.7%(72/84)患者肝功能分级为Child Pugh A,其余为Child Pugh B。81.0%(68/84)患者为BCLC C期,其余为BCLC B期。42例肝外转移患者中,肺转移29例,淋巴结转移14例,骨转移5例,腹膜转移3例,肾转移1例,肾上腺转移1例。
在本队列中,31例HCC患者有TO≥50%, 30例HCC患者有Vp4侵犯,12例HCC患者两者都有。与TO<50%患者相比,TO≥50%患者Child Pugh B级的比例更高(p = 0.021)。Vp4侵犯患者比Vp4未侵犯患者年轻(p = 0.005)。54例Vp4未侵犯的患者中,Vp3侵犯37.0% (20/54),Vp2侵犯7.4%(4/54),无大血管侵犯55.6% (30/54)。

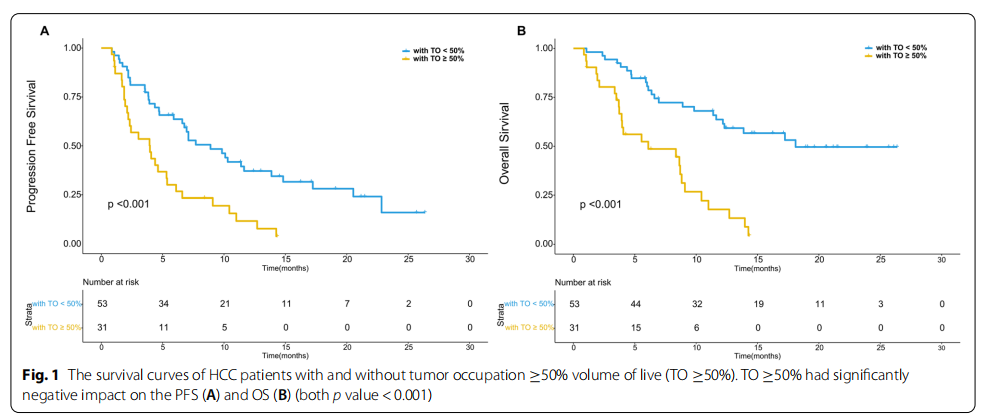
中位随访时间为17.12个月(Vp4浸润组为16.25个月,Vp4未浸润组为18.93个月,TO≥50%组为14.33个月,TO<50%组为18.93个月)。随访期间,76.2%(64/84)患者出现进展,中位无进展生存期(PFS)为6.6个月(95%CI 4.3-8.9个月)。中位OS为11.4个月(95%CI, 7.9-14.9个月)。ORR为20.2% (17/84)。TO≥50%患者的ORR明显低于TO<50%患者(p = 0.016)。Vp4有无有无侵犯患者的ORR差异无统计学意义(p = 0.278)。
TO≥50%患者的中位PFS明显低于TO<50%患者(p<0.001)。TO<50%患者的中位OS为18.1个月,明显长于TO≥50%患者的6.1个月(p<0.001)。TO<50%患者和TO≥50%患者的1年生存率分别为60.7%和42.5%。
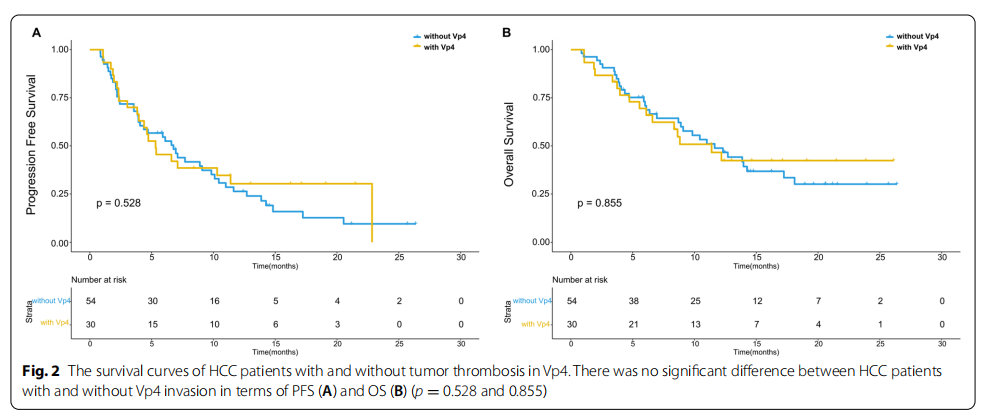
相反,Vp4侵犯与未侵犯患者之间中位PFS无显著差异(p = 0.528)。Vp4未侵犯患者的中位OS为11.63个月,Vp4侵犯患者的中位OS为11.39个月,同样没有统计学差异(p=0.855)。Vp4无侵犯组1年生存率为56.9%,Vp4有侵犯组为54.5%。
多因素分析后,TO≥50%是PFS和OS的独立预测因子(p<0.001)。

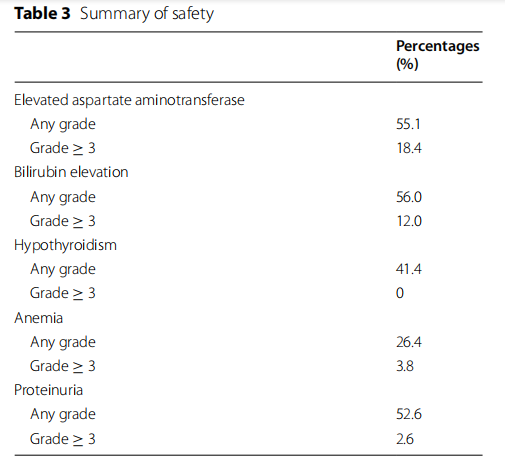
任何级别最常见的AEs为胆红素升高(56.0%)、天冬氨酸转氨酶升高(55.1%)和蛋白尿(52.6%)。任何一种AEs与TO≥50%和Vp4侵犯均无显著相关性。
综上,研究表明,仑伐替尼联合PD-1抑制剂可为晚期HCC伴有Vp4患者带来生存获益。
原始出处:
Sun X, Zhang Q, Mei J, Yang Z, Chen M, Liang T. Real-world efficiency of lenvatinib plus PD-1 blockades in advanced hepatocellular carcinoma: an exploration for expanded indications. BMC Cancer. 2022 Mar 19;22(1):293. doi: 10.1186/s12885-022-09405-7. PMID: 35305593.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#肝细胞#
57
#BMC#
54
#抑制剂#
55
#细胞癌#
42
#PD-1抑制剂#
54
#真实世界#
51
#晚期肝细胞癌#
42
#学习#学习了
50
学习了,谢谢
53
#学习#学习了
68