Front Oncol:神经侵犯是淋巴结阴性结肠癌的预后指标而不是辅助化疗的预测指标
2021-10-30 yd2015 MedSci原创
研究表明,阳性神经侵袭(PNI)是I和II期结肠癌患者的较差的预后指标。但是其不死淋巴结阴性结肠癌患者辅助化疗的预测指标。
结肠癌是常见的恶性肿瘤之一。目前,结肠癌的临床治疗和预后预测标准主要基于AJCC提出的TNM分期。根据NCCN的临床指南,III期结肠癌需要进行辅助化疗以获得更好的预后。然而,TNM分期不足以预测淋巴结阴性(I/II期)结肠癌患者的预后。除了直接生长外,肿瘤细胞还可以通过血液和淋巴通道扩散或沿神经生长。因此,阳性神经侵袭(PNI)被定义为在神经组织内或周围扩散和/或沿神经鞘扩散,甚至在没有淋巴血管侵袭(LVI)或淋巴结转移的情况下。广泛报道PNI的存在提示结直肠癌具有更强的临床病理特征,导致预后较差。已有研究发现PNI可以作为结肠癌接受化疗的指标。PNI对结直肠癌的预后价值已被广泛认识,但其对接受辅助化疗的预测作用尚不明确。近期,Frontiers in Oncology杂志上发表了相关研究,旨在验证PNI对淋巴结阴性结肠癌辅助化疗的预后价值,并评估其对辅助化疗的预测价值。
研究筛查2010年1月1日至2015年12月31日期间SEER数据库中登记的诊断为结肠癌的患者。采用卡方分析评估PNI阴性(PNI(-))组和PNI阳性(PNI(+))组患者的不同人口统计学和临床特征。构建单变量和多变量Cox比例风险回归模型,以检验人口统计学和临床特征以及生存结局。
共从SEER数据库中提取满足纳入和排除标准的淋巴结阴性结肠癌患者57255例。在整个队列中,25450例(44.5%)患者被诊断为I期,21090例(26.8%)患者年龄小于65岁,28369例(49.5%)患者为女性,2372例(4.1%)患者被诊断为PNI。最后一次随访时,存活患者的中位随访时间为37个月。
研究比较PNI(-)组和PNI(+)组患者的不同人口学和临床特征。发现更高T分期(T1期:4.4% VS. 24.7%, T2期:9.2% VS. 21.1%, T3期:62.4% VS. 46.4%, T4期:23.9% VS. 7.8%, P<0.001),诊断年份较晚(2010年为13.7 VS. 16.4%, 2011年为15.4% VS. 16.7%, 2012年为17.5% VS. 16.9%,2013年18.0% VS. 16.6%, 2014年17.5% VS. 16.7%, 2015年17.8% VS. 16.7%, P = 0.003);更高的肿瘤分级(I级为4.9% VS. 10.9%, II级为68.7% VS. 73.0%, III级为21.3% VS.10.1%, IV级为3.7% VS. 2.1%, P<0.001);腺癌93.3% VS. 92.2%,粘液/印戒细胞癌6.7% VS. 7.8%, P = 0.042); 更多的淋巴结检查(10.9% VS. 19.1%小于12个淋巴结检查,89.1% VS. 80.9%大于12个淋巴结检查,P<0.001)更可能与PNI相关。此外,PNI的存在更可能与接受化疗有关(P<0.001)。PNI(−)组和PNI(+)组在诊断时的年龄、种族和性别之间的差异没有达到统计学意义(P>0.05)。
生存分析显示,在I期结肠癌中,PNI(+)患者的5年肿瘤特异性生存(CSS)率为93.6%,)而PNI(-)患者的5年CSS率为96.2%,有显著统计学差异(P = 0.025)。在II期结肠癌患者中, PNI(+)患者的5年CSS率为77.5%,PNI(-)患者的5年CSS率为87.9%,统计学差异进一步扩大(P<0.0001)。
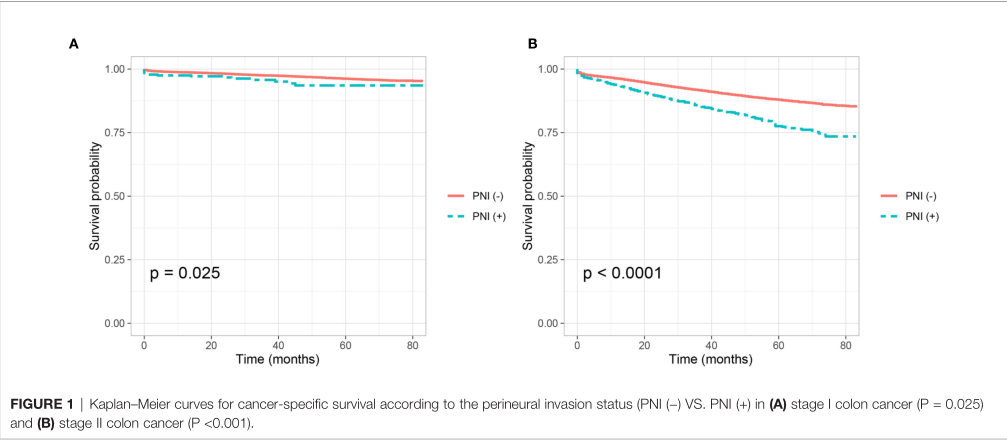
I和II期结肠癌有无神经浸润CSS对比
多因素生存分析显示,对其他预后因素调整后,对于I期结肠癌患者,PNI(+)患者较PNI(-)患者的肿瘤特异性死亡风险增加59% (HR = 1.590, 95%CI = 0.951–2.658, P =0.077)。而对于II期结肠癌患者,PNI(+)患者较PNI(-)患者的肿瘤特异性死亡风险增加60.7% (HR = 1.607, 95%CI = 1.426–1.812, P <0.001)。
研究进一步研究PNI(+)对于II期结肠癌患者的辅助化疗预测作用。T3期PNI(-)结肠癌患者中,接受辅助化疗患者的5年CSS率高于未接受辅助化疗的患者,分别为91.1%和90.0%,差异有统计学意义(P = 0.004);同样,T3期PNI(+)结肠癌患者中,接受辅助化疗患者的5年CSS率高于未接受辅助化疗的患者,分别为83.6%和81.4%,但差异没有达到统计学意义(P = 0.096)。
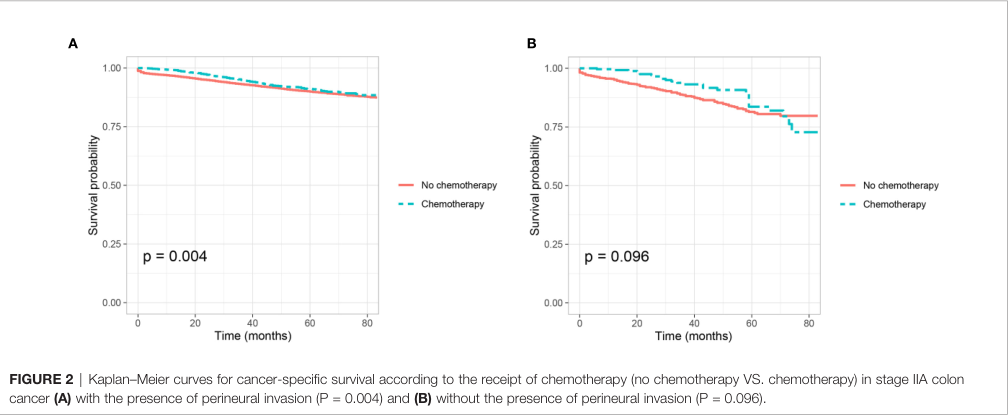
T3期患者有无化疗对CSS影响
多因素分析,接受辅助化疗都不是T3期结肠癌患者无神经浸润(PNI(-))(HR = 0.943,95%CI = 0.802–1.108, P = 0.473)以及有神经浸润(PNI(+)(HR = 0.927, 95%CI = 0.613–1.400, P = 0.717)的独立预后因素。
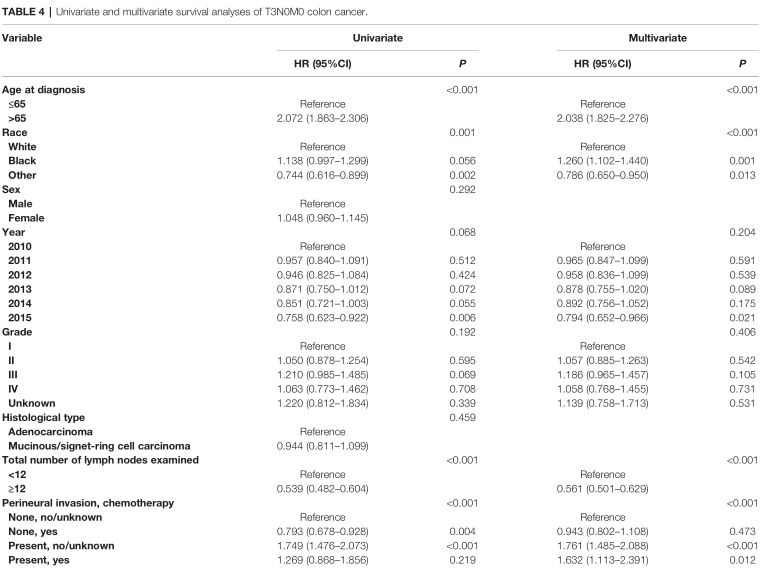
T3期患者预后相关因素
T4期PNI(-)结肠癌患者中,接受辅助化疗患者的5年CSS率高于未接受辅助化疗的患者,分别为80.1%和71.2%,差异有统计学意义(P <0.0001);同样,T4期PNI(+)结肠癌患者中,接受辅助化疗患者的5年CSS率高于未接受辅助化疗的患者,分别为73.3%和62.7%,差异有统计学意义(P = 0.001)。

T4期患者有无化疗对CSS影响
多因素生存分析显示,对其他预后因素调整后,对于T4期PNI(-)结肠癌患者,接受化疗患者较未接受化疗患者的肿瘤特异性死亡风险降低34% (HR = 0.660, 95%CI = 0.559–0.779,P <0.001)。而对于T4期PNI(+)结肠癌患者,接受化疗患者较未接受化疗患者的肿瘤特异性死亡风险降低36.0% (HR = 0.640, 95%CI = 0.438–0.935, P =0.021)。
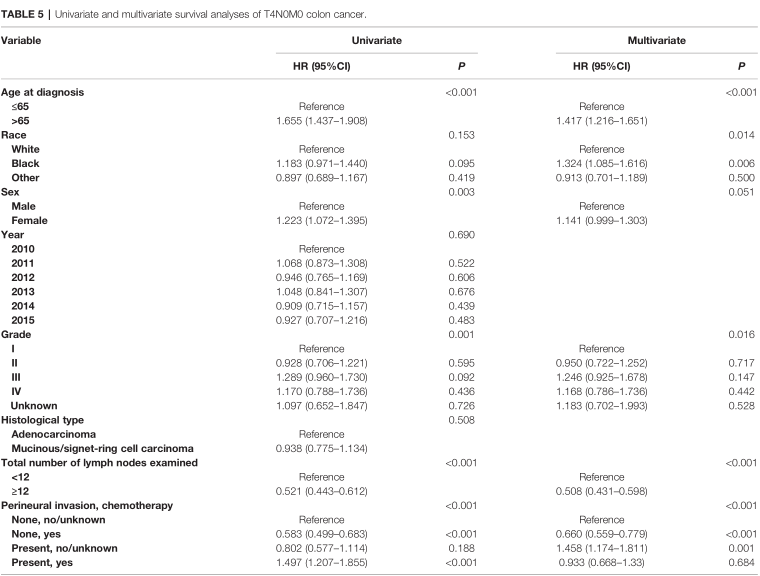
T4期患者预后相关因素
综上,研究表明,阳性神经侵袭(PNI)是I和II期结肠癌患者的较差的预后指标。但是其不死淋巴结阴性结肠癌患者辅助化疗的预测指标。
原始出处:
Tu J, Yao Z, Wu W, Ju J, Xu Y and Liu Y (2021) Perineural Invasion Is a Strong Prognostic Factor but Not a Predictive Factor of Response to Adjuvant Chemotherapy in Node- Negative Colon Cancer. Front. Oncol. 11:663154. doi: 10.3389/fonc.2021.663154
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Oncol#
30
#淋巴结阴性#
28
#淋巴结#
29
#预后指标#
39
#预测指标#
31