肺动脉高压患者的远程6分钟步行试验:是否需要进一步验证?
2022-05-28 刘少飞 MedSci原创
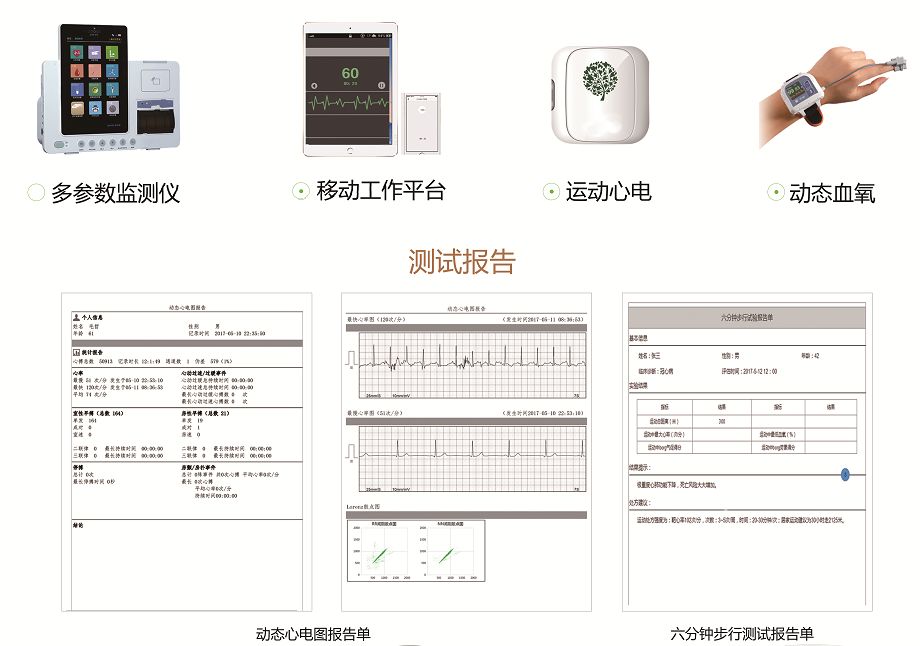
肺动脉高压(PAH)是一种相对罕见的心肺血管疾病,六分钟步行测试(6MWT)可以了解慢性肺部疾病患者的功能状况、疾病严重程度和治疗效果。PAH患者的远程6分钟步行试验:是否需要进一步验证?
六分钟步行测试(6MWT)可以了解慢性肺部疾病患者的功能状况、疾病严重程度和治疗效果。在COVID-19大流行期间,加快了对数字技术使能的医疗保健规定的需求,以减轻病人在诊所的就诊。因此,LaPatra等人在4月1日出版的《美国呼吸与危重症医学杂志》上关于在非临床环境下对肺动脉高压(PAH)或慢性血栓栓塞性PH(CTEPH)进行 "远程 "6MWT的可行性、安全性和准确性的报告是及时和有希望的。使用并结合研究参与者选择的地点 研究参与者选择的地点,研究人员的视听指导,以及对每个参与者的陪伴 "支持",作者发现诊所内与远程设置之间的平均6MWT距离(6MWD)"没有系统差异",诊所内与远程行走之间具有很好的一致性。
除一名患者外(头晕、耳鸣),远程行走期间没有不良事件报告。然而,作者确实发现,在远程行走期间,戴面具的参与者与未戴面具的参与者相比,6MWD较低(约20米)。虽然承认他们的研究结果需要复制,但作者得出结论,远程6MWTs在稳定的PH患者中可能是可行和有效的。我们对作者的工作表示赞赏;然而,他们的结论中有两个方面值得进一步考虑。
观察到口罩与6MWD的下降有关(远程设置),作者建议,当口罩与6MWD相关时,可能需要重复进行无口罩的研究。作者建议,当口罩与临床6MWD的减少有关时,可能需要进行重复的、无口罩的研究。诊室内6MWD的减少。然而,最近我们发现,戴口罩对动脉血氧饱和度、血压和血糖没有影响。对动脉血氧饱和度、对运动的感知反应或45名第一组的6MWD没有影响。PAH患者的临床表现,这与健康人和那些有 肺部疾病。尽管不清楚原因,但戴口罩对6MWD的影响可能在临床上有所不同。6MWD的影响可能在诊所与远程环境中有所不同。基于现有的证据,我们将目前,我们不赞成在门诊环境中不戴口罩与戴口罩的情况下重复6MWT。
第二,LaPatra等人认为,戴口罩对6MWD有负面影响,但 6MWD在诊所和远程环境中没有区别。然而,对数据进行仔细检查后发现 约10名患者(40%的队列)的6MWD相差≥50米,约5名患者(20%的队列)的6MWD相差≥100米。诊所内与偏远地区相比,6MWD相差≥50米(占队列的40%),5名患者相差≥100米(占队列的20%)。
相比之下,使用口罩与不使用口罩的6MWD的差异是≥50米和≥100米。相比之下,只有约5名(占队列的23%)和约2名(占队列的9%)患者戴口罩和不戴口罩的6MWD差异≥50米和≥100米。分别。6MWD的Deming回归拟合与完美一致性线的比较 诊所内与远程环境的Deming回归拟合表明,6MWD距离较短的患者在诊所内 "表现更好 而6MWD较长的患者在远程环境中 "表现更好"。这并不 对于带口罩的6MWD与不带口罩的6MWD来说,情况似乎并非如此,数据点在完全一致线附近的聚集情况更好。
围绕着完全一致的线,出现了若干个问题:1) 运动能力较低的患者(可能是患病的患者)在斜面步行测试中的表现是否更好;2)尽管在诊所与远程环境中,小组的平均6MWD没有差异,但是否会有大量的个体内部差异?2)尽管在诊所和远程环境下,小组平均6MWD没有差异,但在倾斜和远程6MWT之间的一致性方面是否存在大量的个体内异质性?推测性地讲,有可能是病情较重、损伤较大的患者 在临床环境中 "表现得更好",因为有医护人员的直接监督。使得基于远程的6MWT在这些人身上不太合适。此外,鉴于6MWD 差异≥50米,我们认为基于远程的6MWT的适用性不大。我们建议远程6MWT作为功能状态、疾病严重程度和治疗效果的准确和有效标记的适用性。我们认为,远程6MWT作为功能状态、疾病严重程度和疗效的准确有效标志的适用性需要进一步验证。
参考文献:
Helgeson SA, Burger CD, Moss JE, Zeiger TK, Taylor BJ. Remote 6-minute Walk Testing in Patients with Pulmonary Hypertension: Further Validation Needed? Am J Respir Crit Care Med. 2022 May 24. doi: 10.1164/rccm.202204-0762LE. Epub ahead of print. PMID: 35608525.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#步行#
50
#6分钟步行试验#
47
#动脉高压#
41
#肺动脉高压患者#
41
精彩评论,需要您登录查看
47