【一般资料】
患者,男,55岁
【主诉】
因双鼻塞、流脓涕1年余于2016年8月13日入院。
【现病史】
患者1年多前无明显诱因出现双侧鼻腔持续性鼻塞,伴有大量脓涕、嗅觉下降,无明显头痛、头昏、涕中带血、耳闷等。6年前曾在外院行鼻息肉手术,长期有打喷嚏病史,既往无支气管哮喘病史。此次发病以来曾断续接受口服抗生素、鼻炎冲剂、黏液促排剂、鼻喷类固醇激素等药物治疗及鼻腔冲洗治疗2~3个月,症状无明显改善,尤其是鼻塞仍持续加重。来宜兴市人民医院进一步诊治。
【体格检查】
鼻外观无畸形。鼻内镜下见双鼻黏膜慢性充血、肿胀,鼻中隔无明显偏曲,双侧总鼻道大量荔枝肉样新生物堵塞,来源于中鼻道,表面附有大量脓性分泌物,双侧中鼻甲息肉样变,双侧下鼻甲肿胀肥厚,鼻咽部未能窥清。
【辅助检查】
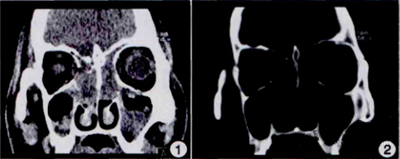
嗜酸性细胞百分比8.25。鼻旁窦CT示:双侧鼻腔软组织影,两侧上颌窦、筛窦、额窦、蝶窦炎症(图1、2)。
【初步诊断】
双鼻息肉;慢性鼻窦炎;变应性鼻炎。
【治疗】
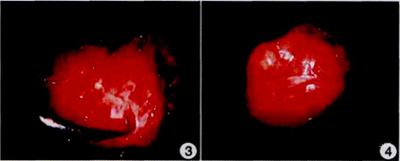
入院后在全身麻醉下行功能性内镜鼻窦手术,术中先以电动切割器切除双鼻息肉,再依次开放双侧上颌窦、筛窦、额窦及蝶窦,窦腔骨壁略硬,骨化尚不明显,窦腔内有大量荔枝肉样新生物及黏脓性分泌物,均仔细清除,术中出血较多,部分区域解剖标志不清。清除左侧额窦口荔枝肉样新生物后见窦口狭窄,试图扩大之,咬除窦口后外方筛顶处一棘突时有较多出血,视野不清,以双极电凝逐步烧灼止血,检查术腔未见活动出血,双鼻腔以可吸收止血绫、气囊等填塞。术毕术者按压双侧眼球,发现左侧眼球硬度明显增高,出现持续加重的肿胀,球结膜充血水肿明显,眶周稍许瘀血。急请眼科会诊,眼科专科检查见两侧瞳孔等大等圆,直接、间接对光反射均正常,右眼球较凸出,球结膜充血水肿,内眦下缘处皮肤瘀血,且眶内压增高,认为有眶内出血可能,建议行眶减压以减轻视神经压迫。故立即继续于全身麻醉下行左鼻腔、鼻窦探查及眶减压术,取出左鼻腔填塞物,探查左鼻腔术区未见明显活动性出血,左侧纸样板尚完整,向内侧突起,以直角尖锐剥离子于纸样板中部起逐步向四周仔细剥除纸样板骨质(图3),直至眶尖部,切开眶骨膜后见黄色眶脂肪暴露凸出(图4),按压左侧眼球,硬度下降,肿胀减轻,达到减压效果。重新检查筛顶,辨别筛前动脉,双极电凝再次烧灼加固止血。术毕,左鼻腔筛窦区未填塞任何材料,总鼻道予少许明胶海绵阻挡渗血。术后除常规予抗炎、止血和护胃等治疗外,予甲基强的松龙200mg、20%甘露醇250ml每日1次静脉滴注,共3d。术后3d抽出鼻腔填塞物,检查术腔见左侧筛窦区少许血痂,予以清除,见眶脂肪未受明显压迫,左眼睑肿胀减轻,球结膜仍充血,内眦稍有瘀血,眼球运动正常,视物清晰。术后7d,左眼上下睑肿胀均基本消退,内眦瘀血及球结膜充血均减轻,眼球运动正常,视物清晰。术后3周,左眼睑肿胀及内眦下缘皮肤瘀血完全消退,球结膜稍充血,双眼球运动正常,眼科检查视力正常,无复视。随访半年,患者左眼无明显复视、视力下降。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#复发性#
0
#血肿#
24
#紧急#
25
学习一下谢谢
45
学习
58
优质资源.共同学习
43