Nat Commun:揭示巨噬细胞活化与肿瘤进展相关的调节机制
2018-07-04 胖胖同学 iNature
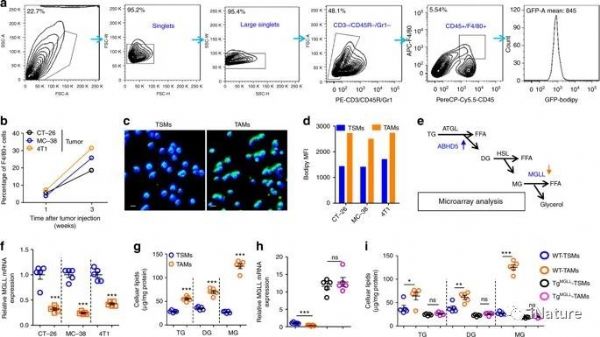
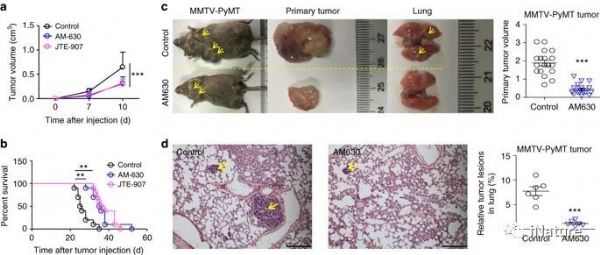
2018年7月3日,第三军医大学缪洪明课题组、梁后杰课题组、李咏生课题组与南方医科大学等研究人员合作在Nature Communications上在线发表了题为“Monoacylglycerol lipase regulates cannabinoid receptor 2-dependent macrophage activation and cancer progression"的研究论文。研
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#肿瘤进展#
40
#Nat#
41
#COMMUN#
35
#调节机制#
43
巨噬细胞活化与肿瘤进展相关.
72
好好学习天天向上认真学习
53
学习了谢谢分享
61