Lancet Oncol:马骏教授团队研究出提高鼻咽癌疗效新方法
2016-11-06 中山大学肿瘤防治中心 中山大学肿瘤防治中心
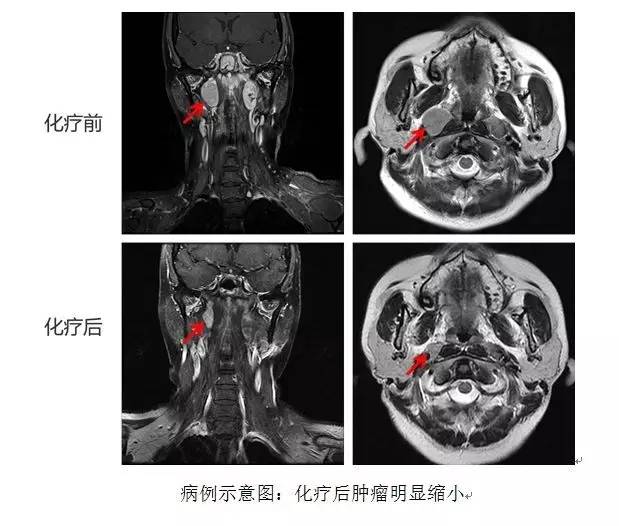
中山大学附属肿瘤医院马骏教授团队牵头四川大学华西医院、佛山市第一人民医院、华中科技大学同济医院等10个临床研究中心共同开展了一项三药联合化疗方案(多西他赛+顺铂+5-氟尿嘧啶,简称TPF)治疗局部晚期鼻咽癌的大型前瞻性Ⅲ期临床试验(研究号NCT01245959),首次证实该方法有效。研究结果于近日在全球顶级肿瘤专业杂志《柳叶刀肿瘤》在线发表(2015年影响因子26.5分)
中山大学附属肿瘤医院马骏教授团队牵头四川大学华西医院、佛山市第一人民医院、华中科技大学同济医院等10个临床研究中心共同开展了一项三药联合化疗方案(多西他赛+顺铂+5-氟尿嘧啶,简称TPF)治疗局部晚期鼻咽癌的大型前瞻性Ⅲ期临床试验(研究号NCT01245959),首次证实该方法有效。研究结果于近日在全球顶级肿瘤专业杂志《柳叶刀肿瘤》在线发表(2015年影响因子26.5分)。
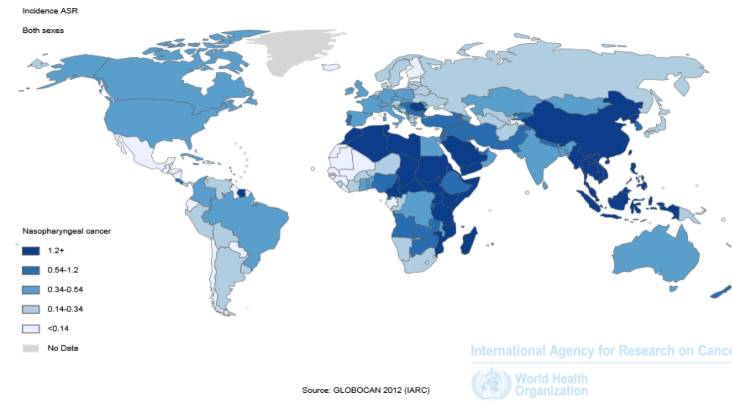
中国的鼻咽癌发病率居世界之冠,据世界卫生组织统计,全球40%的鼻咽癌发生在中国,其中以广东最多,因此鼻咽癌也被称为“广东瘤”,以中山大学附属肿瘤医院统计数据为例,2015年全年收治新发鼻咽癌病例达4703例。由于鼻咽癌发病部位隐蔽,初次到医院就诊的患者中70%以上已经伴有周围颅骨侵犯和颈部淋巴结转移,治疗效果差。如何提高这部分局部区域晚期患者的治疗效果,一直以来都是全世界学者的研究重点。
“先放疗后化疗”无助患者受益
早在2006年,在中山大学5010临床研究项目的支持下,马骏教授团队就发现国际指南推荐的同期放化疗后给予强化的3个疗程的辅助化疗(双药方案顺铂+5-氟尿嘧啶,简称PF)不适于中国人,不能提高疗效反而增加了患者的痛苦和经济负担,研究成果于2012年发表于《柳叶刀肿瘤》。“一石激起千层浪”,文章发表当年,欧洲指南就迅速做出回应,采纳了该研究结果。次年美国指南也做出了相应修订,开始全球推广应用。



马骏教授团队在查房及病例讨论
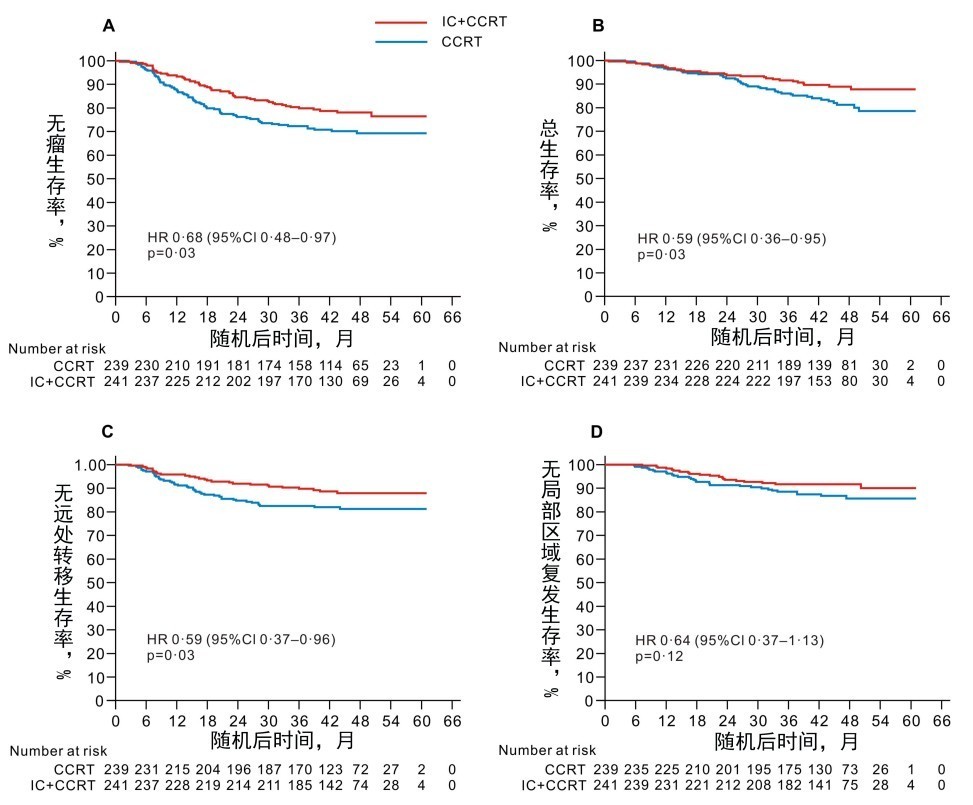
生存曲线图
(CCRT:同期放化疗组;IC+CCRT:诱导+同期放化疗组)
新方案有望被国际指南采纳
该研究是近10年来,在优化局部晚期鼻咽癌化疗方案的试验中,唯一的一个可同时降低远处转移率并提高患者总生存率的三期临床试验,极大地推动了局部区域晚期鼻咽癌放化综合治疗的进展。TPF诱导化疗序贯同期放化疗有望被国际指南采纳,成为局部区域晚期鼻咽癌的标准治疗方案。
《柳叶刀肿瘤》同期述评本研究成功要点
受益人群的精准选择:相对于其他几项类似的研究,本研究中排除了局部区域晚期患者中无区域淋巴结转移(T3-4N0)的这一低远转风险的亚组,更精准的聚焦于高远转风险的人群,避免了“过度治疗”。
有效方案的精准选择:传统的PF方案是有效的,但是强度仍不够,多西他赛是一种紫杉烷类抗癌植物药,与PF联合(TPF方案)具有协同作用。研究显示TPF较PF诱导化疗可以显著提高其他头颈部肿瘤患者的总生存率。本研究选择了TPF这一有效的诱导化疗方案是患者生存获益的关键因素。
参与单位通力协作完成的大样本三期临床研究:来自8个省份10所肿瘤治疗中心(中山大学附属肿瘤医院、四川大学华西医院、佛山市第一人民医院、华中科技大学同济医院、北京大学肿瘤医院、浙江省肿瘤医院、江西省肿瘤医院、广西医科大学附属肿瘤医院、复旦大学附属肿瘤医院、哈尔滨医科大学附属第三医院)的480例病例,严谨的数据,使得诱导化疗的效果得以体现。
严谨规范的研究实施:严格遵循国际CONSORT标准(临床试验报告的统一标准)的22项要求,逐一对照地设计、实施、以及报告此项临床试验,使得本研究的质量得到明显提高。

由我中心牵头全国10家医疗中心参与本项临床试验
院所在1964年成立之初,即将“广东瘤”——鼻咽癌这一严重危害华南地区人民健康的恶性肿瘤锁定为研究与攻克的对象,一代代学人薪火相传,不畏艰辛,求索不止,在基础和临床研究方面步步前行,在鼻咽癌的发病风险预测、预防方面取得了显著成效,推动鼻咽癌临床诊疗进入个体化精准诊疗时代。
中山大学肿瘤防治中心(附属肿瘤医院、肿瘤研究所)鼻咽癌研究成果
1962年
首任所长梁伯强教授在院所筹建时期首次在国际上提出鼻咽癌病理分型(三类六型),成为鼻咽癌病理分型的国际标准;同年,在莫斯科第八届国际肿瘤大会上首次提出鼻咽癌组织学分类。
主要完成人:梁伯强教授
1964年
首任院长谢志光教授等人探索晚期鼻咽癌病人的有效治疗方法,实施“压腹阻断腹主动脉循环,腔静脉注入氮芥疗法”(简称“半身化疗”),疗效显著。
主要完成人:谢志光、李振权、闵华庆、钟国华等
1978年
“鼻咽癌的防治研究”荣获全国科学大会奖
主要完成人:肿瘤研究所、肿瘤医院、中山医学院基础学院、卫生统计教研组
1978年
“中国南方五省鼻咽癌流行病学的初步调查研究” 荣获全国科学大会奖
主要完成人:闵华庆等
1978年
“鼻咽癌的放射治疗”荣获全国医药卫生科学大会奖
主要完成人:潘国英、曾其祥、毛志达、张恩罴、梁培根
1983年
主编《鼻咽癌临床与实验研究》获第三届全国优秀科技图书一等奖
主要完成人:李振权、潘启超、陈剑经
1992年
鼻咽癌新分期方案被中华放射肿瘤学会命名为“92分期”
主要完成人:闵华庆、洪明晃、马骏
“鼻咽癌防治系列研究”获国家科技进步二等奖
主要完成人:闵华庆、黄腾波、洪明晃
2002年
定位并鉴定了鼻咽癌家族性遗传易感基因,研究成果发表于顶级国际期刊《Nature Genetics》,并获同年的中国高等学校十大科技进展
主要完成人:曾益新、冯炳健
2005年
完成首株鼻咽癌来源的EB病毒全序列分析
主要完成人:曾益新、曾木圣
2005年
“鼻咽癌分子遗传学研究”获国家自然科学二等奖
主要完成人:曾益新、方嬿、邵建永
2007年
有关鼻腔/口咽侵犯归为T1亚期,咽后淋巴结转移归为N1a的两项研究结果被第七版AJCC/UICC分期采纳
主要完成人:马骏、刘孟忠、唐玲珑、毛燕萍
2009年
“基于现代影像技术的鼻咽癌综合治疗临床研究”获得国家科技进步二等奖
主要完成人:马骏、罗伟、孙颖
2010年
发现了多个散发性鼻咽癌易感基因,研究成果发表于顶级国际期刊《Nature Genetics》
主要完成人:曾益新、贝锦新
2011年
同期化疗可以提高中期鼻咽癌的疗效,研究成果发表于JNCI,并被欧洲EHNS-ESMO- ESTRO指南采纳
主要完成人:麦海强、陈秋燕、温月凤、郭灵、刘怀
2012年
有关“辅助化疗不能在同期放化疗基础上进一步提高局部区域晚期鼻咽癌生存”的研究结果在Lancet Oncology上发表,研究方案改变了欧洲EHNS-ESMO- ESTRO指南和美国NCCN指南
主要完成人:马骏、陈磊、胡超苏、陈晓钟
2012年
miRNA分子标签的研究结果发表于Lancet Oncology ,“鼻咽癌放化综合治疗及个体化治疗基础的研究”研究成果入选中国高等学校十大科技进展
主要完成人:马骏、陈磊、柳娜
2015年
“鼻咽癌诊疗关键策略研究与应用”项目荣获国家科技进步二等奖
主要完成人:马骏、赵充、麦海强
2015年
全球首个鼻咽癌风险预警芯片,投入临床使用
主要完成人:曾益新、邵建永
2016年
全球第一项关于复发转移鼻咽癌临床研究成果在全球顶级杂志The Lancet发表
主要完成人:张力、黄岩、洪少东、杨云鹏
2016年
发现了两个新的鼻咽癌易感基因(TERT/CLPTM1L和CIITA),成果发表于《人类分子遗传学》(Human Molecular Genetics)
主要完成人:曾益新 贝锦新
2016年
TPF诱导化疗可以提高局部晚期鼻咽癌生存率的研究成果发表于Lancet Oncology
主要完成人:马骏、孙颖、李文斐、陈念永、张宁、胡国清、谢方云、孙艳
马骏(通讯作者):中山大学肿瘤防治中心放疗科教授、主任医师、博士生导师、鼻咽癌放疗科首席专家。现任中山大学附属肿瘤医院常务副院长。长期从事鼻咽癌的放化综合治疗和个体化治疗。
孙颖(共同第一作者):中山大学肿瘤防治中心放疗科主任医师、博士生导师。现任中山大学附属肿瘤医院院长助理。主要研究方向为鼻咽癌精确放疗及正常组织保护。
李文斐(共同第一作者):中山大学肿瘤防治中心放疗科主治医师、博士。主要研究方向为鼻咽癌放疗及综合治疗。
陈念永(共同第一作者):四川大学华西医院肿瘤中心教授、主任医师、博士生导师、医院一级岗位专家。现任四川大学华西医院肿瘤中心主持工作副主任、华西临床医学院肿瘤学教研室主任。长期从事肿瘤尤其是头颈部肿瘤、及淋巴瘤的放化疗综合治疗和个体化精准医疗。
张宁(共同第一作者):佛山市第一人民医院放疗科主任医师。现任佛山市第一人民医院鼻咽放疗科主任。主要研究领域是鼻咽癌等恶性肿瘤的放射治疗。
胡国清(共同第一作者):华中科技大学同济医院肿瘤中心教授、主任医师、博士生导师。主要专长和研究领域是肿瘤的放疗及其综合治疗,尤其是在鼻咽癌等头颈肿瘤的放疗。
谢方云(共同第一作者):中山大学肿瘤防治中心放疗科教授、主任医师、硕士生导师。主要研究方向是头颈部肿瘤放疗,特别是鼻咽癌综合治疗。
孙艳(共同第一作者):北京大学肿瘤医院,医学博士、主任医师、硕士生导师,头颈放疗负责人。主要研究方向是头颈肿瘤的综合治疗、放化疗不良反应评估及治疗、靶向治疗及基因治疗。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#马骏教授#
0
#Lancet#
35
#新方法#
32
#马骏#
47
鼻咽癌先化疗后放疗成新的突破口
75
#Oncol#
22
在优化局部晚期鼻咽癌化疗方案的试验中,唯一的一个可同时降低远处转移率并提高患者总生存率的三期临床试验,极大地推动了局部区域晚期鼻咽癌放化综合治疗的进展。TPF诱导化疗序贯同期放化疗有望被国际指南采纳,成为局部区域晚期鼻咽癌的标准治疗方案。
67
再次领略团队的色彩
55
有点滞后的新闻
57
这篇咨询不错哦,值得学习,对于临床工作和科研思路都很有帮助。
59