Sci Transl Med:基于一种靶向质谱的高通量技术快速验证潜在的癌症标记分子
2012-07-23 ZinFingerNase 生物谷
来自瑞士苏黎世联邦理工学院的研究人员开发出一种方法来测试癌症生物标记分子的临床意义。这种方法能够显著性地加快实验室发现的癌症标记物的应用。 由于蛋白质组和基因组研究以及利用计算机为生物过程建模上取得的巨大进展,研究人员在最近几年已发现一千多种潜在的蛋白生物标记分子。生物标记分子的候选物名单也变得越来越长。然而,在文献中提出和记录的大多数蛋白生物标记分子并没有用于临床应用中。将人们开发出的新生物标

来自瑞士苏黎世联邦理工学院的研究人员开发出一种方法来测试癌症生物标记分子的临床意义。这种方法能够显著性地加快实验室发现的癌症标记物的应用。
由于蛋白质组和基因组研究以及利用计算机为生物过程建模上取得的巨大进展,研究人员在最近几年已发现一千多种潜在的蛋白生物标记分子。生物标记分子的候选物名单也变得越来越长。然而,在文献中提出和记录的大多数蛋白生物标记分子并没有用于临床应用中。将人们开发出的新生物标记分子用于临床没有取得进展的主要原因是缺乏一种验证大多数生物标记分子候选物的方法。
根据于2012年7月11日发表在Science Translational Medicine期刊上的一篇论文,论文第一作者Ruth Hüttenhain和Martin Soste开发出一种策略来大规模地和快速地测量潜在的生物标记分子以及验证它们的临床用途。这种方法基于一种靶向质谱的高通量技术,能够以一种可靠且可重现的方式在特定时间点上确定存在于生物样品中的蛋白。
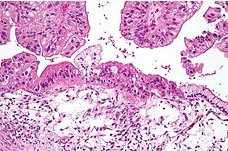
在他们的研究中,研究人员利用开发出的方法来检测1157个潜在的生物标记分子:检测它们在不同人癌组织中的丰度变化,哪些与促进癌症产生的突变基因相关联。研究人员最终在来自癌症病人和健康个人的血液样品和尿液样品中测试他们的检测方法。他们能够在血清中检测180多种不同的生物标记分子,而且检测浓度极限为每毫升血清十亿分之一克。在尿液样品中,研究人员发现400多种不同的蛋白生物标记分子。利用这种方法,潜在性生物标记分子名单能够被快速地和有效地缩短。尽管这些检测不能直接用于癌症诊断,但是它们能够缩短基础研究与临床应用之间的差距。
在对卵巢癌的识别研究中,研究人员证实他们的方法是有效的:它能够验证血清中存在的潜在生物标志分子。为此,研究人员不仅可以测量文献中描述过的生物标记分子候选物,而且也能测量基于基因组数据的计算模型预测出的新的生物标记分子。因此,这些研究结果强调了这种质谱分析方法验证新的蛋白生物标记分子的巨大潜力。这项研究还描述了癌症、基因数据和确定病人急性状态的蛋白质组测量结果之间存在的联系。总之,这种新方法能够被用来验证所有病人样品中的潜在生物标记分子候选物,而且开发针对疾病相关蛋白的高度特异性验证方法的策略也能够被应用于其他疾病。(生物谷:Bioon.com)
本文编译自Cancer biomarkers re-evaluated

doi: 10.1126/scitranslmed.3003989
PMC:
PMID:
Reproducible Quantification of Cancer-Associated Proteins in Body Fluids Using Targeted Proteomics
Ruth Hüttenhain1,2,*,†, Martin Soste1,*, Nathalie Selevsek1, Hannes Röst1,3, Atul Sethi1,3, Christine Carapito1, Terry Farrah4, Eric W. Deutsch4, Ulrike Kusebauch4, Robert L. Moritz4, Emma Niméus-Malmström5, Oliver Rinner6 and Ruedi Aebersold
The rigorous testing of hypotheses on suitable sample cohorts is a major limitation in translational research. This is particularly the case for the validation of protein biomarkers; the lack of accurate, reproducible, and sensitive assays for most proteins has precluded the systematic assessment of hundreds of potential marker proteins described in the literature. Here, we describe a high-throughput method for the development and refinement of selected reaction monitoring (SRM) assays for human proteins. The method was applied to generate such assays for more than 1000 cancer-associated proteins, which are functionally related to candidate cancer driver mutations. We used the assays to determine the detectability of the target proteins in two clinically relevant samples: plasma and urine. One hundred eighty-two proteins were detected in depleted plasma, spanning five orders of magnitude in abundance and reaching below a concentration of 10 ng/ml. The narrower concentration range of proteins in urine allowed the detection of 408 proteins. Moreover, we demonstrate that these SRM assays allow reproducible quantification by monitoring 34 biomarker candidates across 83 patient plasma samples. Through public access to the entire assay library, researchers will be able to target their cancer-associated proteins of interest in any sample type using the detectability information in plasma and urine as a guide. The generated expandable reference map of SRM assays for cancer-associated proteins will be a valuable resource for accelerating and planning biomarker verification studies.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Transl#
36
#TRA#
25
#高通量#
33
#质谱#
31
#Med#
21