J Thorac Oncol: Lorlatinib(劳拉替尼)治疗既往经治ALK阳性晚期或转移NSCLC中国患者的疗效
2022-03-21 yd2015 网络
研究表明,既往ALK-TKI治疗进展的ALK阳性晚期NSCLC中国人群中,劳拉替尼治疗疗效显著,同时颅内控制率高。
近期,Journal of Thoracic Oncology杂志上发表了一项2期临床研究结果。该研究是一项开放标签、双队列2期临床研究,主要是评估Lorlatinib(劳拉替尼)治疗既往经治ALK阳性晚期或转移NSCLC中国患者的疗效。广东省人民医院吴一龙教授为通讯作者,陆舜教授和周清教授为共同第一作者。

该研究为开放标签、双队列2期临床研究(NCT03909971);ALK-TKI治疗后患者病情进展分为队列1:既往克唑替尼治疗和队列2:既往除克唑替尼外的ALK-TKI治疗),≧1个颅外可测量病灶,ECOG PS为0-2。患者接受口服劳拉替尼100 mg,每日1次,连续21天为一周期。主要终点:根据RECIST 1.1标准,ICR评估在队列1中的客观缓解。
在数据截止时(2020年8月10日),109例患者被纳入(队列1:N = 67;队列2:N = 42)。所有患者均为中国人,其中女性56例(51.4%),男性53例(48.6%)。中位(范围)年龄为51.0(19-77)岁。在队列1中,有4名患者(6.0%)患有IIIB期,1名患者(1.5%)患有IIIC期,62名患者(92.5%)患有IV期。在队列2中,所有患者均为IV期癌症(n = 42;100%)。克唑替尼和塞瑞替尼是常的ALK-TKIs。
队列1患者中,CR,PR,SD和PD各有8、39、8和4例患者,ORR为70.1%(95%CI: 57.7-80.7;p<0.0001;主要终点),中位DOR尚未达到,中位TTR为1.4个月(0.6–11.1)。队列2患者中,CR,PR,SD和PD各有2、18、6和3例患者,ORR为47.6%(95%CI:32.0-63.6;次要终点),中位DOR为11.2个月 (2.9–NR),中位TTR为1.4个月 (1.2–5.6)。

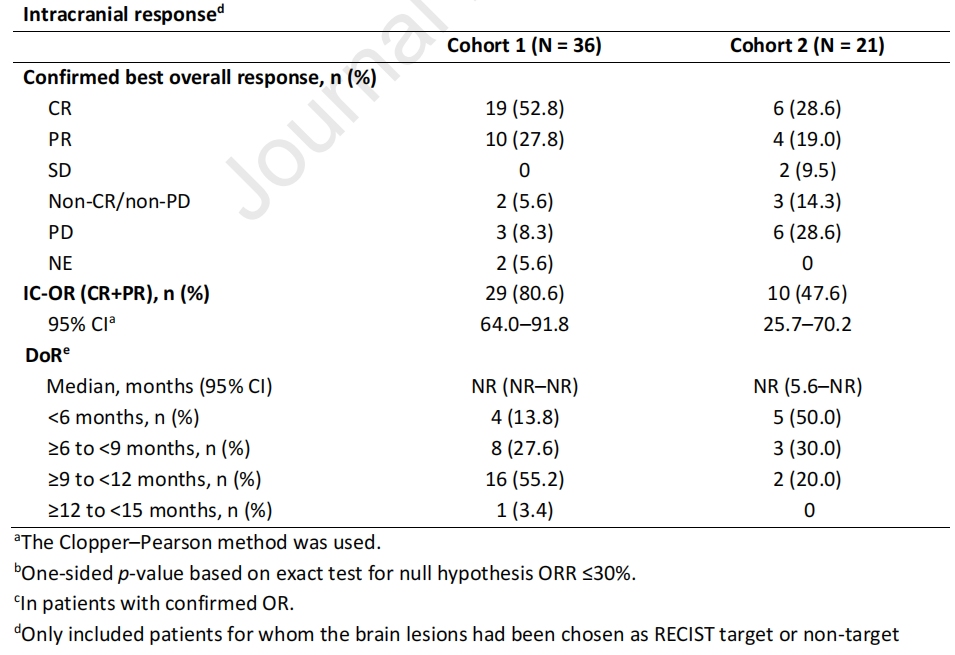
颅内应答评估时,队列1患者中,CR,PR,SD和PD各有19、10、0和3例患者,ORR为80.6%,中位DOR尚未达到。队列2患者中,CR,PR,SD和PD各有6、4、2和6例患者,ORR为47.6%,中位DOR尚未达到。
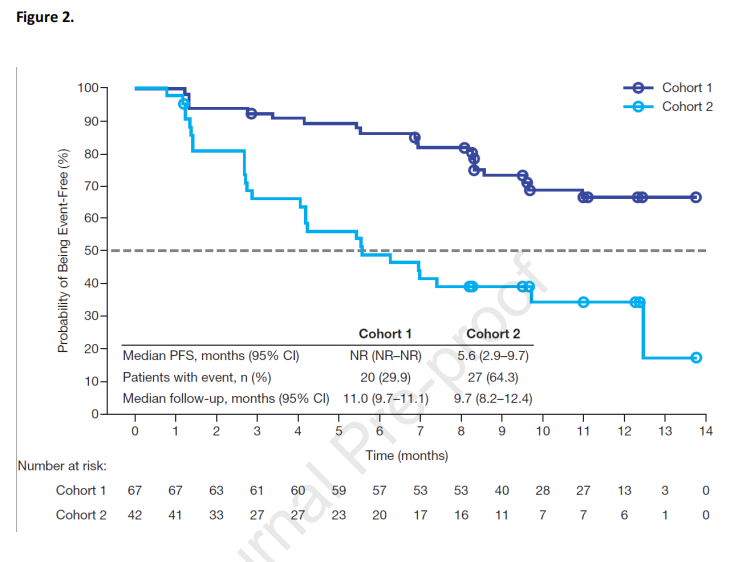
队列1中位无进展生存期(PFS)未达到,12个月PFS率为66.4% (95% CI: 52.4-77.1);队列2中位PFS为5.6个月(95% CI: 2.9–9.7),12个月PFS率为34.2% (95% CI: 19.2-49.8)。两队列的中位OS均未达到。
高胆固醇血症(92.7%)和高甘油三酯血症(90.8%)是常见的治疗相关不良事件(TRAE)。9例(8.3%)患者有严重TRAE;1例患者因为TRAE而永久停止治疗。

综上,研究表明,既往ALK-TKI治疗进展的ALK阳性晚期NSCLC中国人群中,劳拉替尼治疗疗效显著,同时颅内控制率高。
原始出处:
Shun Lu, Qing Zhou, Xiaoqing Liu,et al. Lorlatinib for Previously Treated ALK-Positive Advanced Non-Small Cell Lung Cancer: Primary Efficacy and Safety From a Phase 2 Study in China. Journal of Thoracic Oncology. DOI: https://doi.org/10.1016/j.jtho.2022.02.014
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#THORAC#
47
#ALK阳性#
51
#Oncol#
43