肩锁关节脱位合并喙突骨折及喙锁韧带部分断裂1例
2019-08-18 邓介超 丛云海 姜海军 中国骨与关节损伤杂志
患者,男,43岁,与他人打架时被推倒,右肩着地,然后被重物砸伤右肩。伤后右肩疼痛、肿胀,就诊社区卫生服务中心摄右肩关节正位X线片检查,初步诊断右肩锁关节脱位,并行健侧X线片对比检查。为进一步诊治转至笔者所在医院,临床医师仔细阅片后发现喙突骨折。入院时左手扶右上肢,右肘屈曲并固定于右侧胸壁,右肩因疼痛拒绝活动。琴键征阳性,右侧喙突压痛,无神经及血管损伤。入院后进一步行CT检查,明确诊断喙突骨折。此外
病例报道
患者,男,43岁,与他人打架时被推倒,右肩着地,然后被重物砸伤右肩。伤后右肩疼痛、肿胀,就诊社区卫生服务中心摄右肩关节正位X线片检查,初步诊断右肩锁关节脱位,并行健侧X线片对比检查。为进一步诊治转至笔者所在医院,临床医师仔细阅片后发现喙突骨折。入院时左手扶右上肢,右肘屈曲并固定于右侧胸壁,右肩因疼痛拒绝活动。琴键征阳性,右侧喙突压痛,无神经及血管损伤。入院后进一步行CT检查,明确诊断喙突骨折。此外,X线片可见锁骨远端抬高且喙锁间隙较正常明显增加,提示肩锁韧带及喙锁韧带均断裂,肩锁关节脱位按Rockwood分型为Ⅲ型,喙突骨折按Eyres分型为累及肩胛骨上部的Ⅳ型。排除手术禁忌证并完善术前准备后,行肩锁关节脱位切开复位内固定、喙突骨折撬拨复位空心钉内固定、喙锁韧带缝合术。
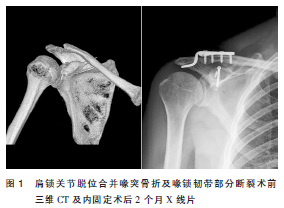
采用全身麻醉,取沙滩椅位,作右肩关节前方切口,逐层切开,沿三角肌、胸大肌间隙分离,剥离三角肌锁骨附着处,于喙突上方切开胸锁筋膜,探查见喙锁韧带锥状束断裂,肩锁韧带断裂并嵌入肩锁关节,肩锁关节脱位。清理肩锁关节并复位,用锁骨钩钢板固定肩锁关节。触摸喙突顶端确认喙突位置后沿喙突走行方向置入2枚克氏针,克氏针深度不超过喙突骨折线,通过克氏针撬拨复位骨折,撬拨过程中沿喙突伸入手指触摸骨折复位情况,直至骨折复位,不需要广泛显露而直视骨折线。复位后将克氏针继续置入固定骨折,置入空心钉导针,沿导针置入空心钉固定。喙锁韧带锥状束用带线锚钉缝合。术后24h拔除切口引流管并复查术后X线片。术后2个月X线片显示骨痂形成,喙突骨折线模糊(图1);右肩关节无明显疼痛,可进行日常活动。
讨论
喙突骨折多发于基底部并且合并肩锁关节脱位。喙突骨折在X线片上极易被肱骨头及肩胛岗的影像重叠而漏诊,可采用向头侧倾斜特定角度投照,减少骨性重叠以清楚显示喙突。出现肩锁关节脱位的患者需警惕喙突骨折,必要时需要行CT检查明确诊断。喙突的位置较深,其周围有胸大肌、三角肌、肩胛骨、肱骨等结构的保护,因此多为直接暴力导致喙突骨折。喙锁韧带、喙肩韧带及胸小肌、联合腱附着于喙突,此外喙突、喙肩韧带及肩峰组成喙肩弓,在整个肩关节的活动和稳定中起到非常重要的作用。当肩关节上部悬吊复合体一处发生损伤对于肩关节整体的稳定性影响不明显,2处或2处以上结构损伤则提示肩关节不稳定,多需要手术治疗。喙突骨折的原因有直接暴力、肩锁关节脱位时喙锁韧带牵拉或喙突附着处肌腱收缩、肩胛盂受撞击引起的肩胛盂和喙突基底部骨折、肱骨头前脱位撞击等。该患者存在肩锁关节脱位、喙锁韧带部分断裂(锥状韧带)及喙突骨折累及肩胛骨上缘。分析该患者受伤机制,考虑第一次摔倒暴力导致肩锁关节脱位及喙锁韧带部分断裂,第二次重物砸伤是引起喙突骨折的直接暴力。
目前尚无针对喙突骨折治疗的随机对照研究,大部分文献为个案或小样本病例报道,其手术指征尚无统一标准。通常认为Eyres分型中Ⅰ、Ⅱ、Ⅲ型骨折采用非手术治疗可取得较好的临床效果。因喙突为多结构附着处,在维持肩关节稳定性方面发挥着重要作用,累及肩胛骨及肩胛盂且明显移位的EyresⅣ、Ⅴ型骨折需手术治疗以维持肩关节稳定性。合并肩锁关节脱位或肩胛盂骨折的患者因肩关节上部悬吊复合体稳定性被破坏也需手术治疗。手术入路多采用前方入路,分离胸大肌、剥离三角肌内侧显露喙突和喙锁韧带。合并肩锁关节脱位时,切口向后上延长显露锁骨远段及肩锁关节。若合并肩峰骨折、肩胛冈骨折及肩胛体骨折需要手术治疗也可采用背侧的肩关节后侧入路。
多数文献报道喙突骨折术中需剥离喙突附着软组织显露骨折并在直视下复位。本例术中未过多剥离喙突附着组织,以血管钳沿喙突小范围钝性剥离,剥离空间为可容一指伸入以触摸喙突骨折线。用克氏针撬拨复位骨折,因喙突为多结构附着处,喙突上附着的软组织在撬拨时可有辅助复位的效果。撬拨过程中手指触摸骨折对位情况,骨折复位后C型臂X线透视确认复位效果。喙突内上方为容纳肩胛上神经的肩胛上切迹,内下方有腋动静脉和臂丛神经经过,手术时尽量避免在其内侧操作,警惕血管神经损伤。在置入撬拨克氏针时需分次逐渐增大进针深度,每次进针后需透视确认深度及位置,避免穿透胸膜造成气胸或偏移到喙突内侧损伤血管神经。撬拨复位法可以尽可能地避免过多软组织损伤并减少骨折端血运破坏。喙突复位后置入1枚空心钉导针固定,透视确认位置,若位置不佳则不必拔除导针,以上枚导针为引导继续调整下一枚导针置入位置及角度,最后沿适宜的导针置入空心拉力螺钉。根据喙突骨折类型和移位情况,文献报道有多种内固定方式,如空心拉力螺钉、松质骨螺钉、克氏针等,目前较为常用的是空心拉力螺钉。Lidgett等采用锚定装置将喙突与锁骨固定以对抗肱二头肌短头及喙肱肌对喙突牵拉导致的向尾侧移位倾向。笔者在术中先复位并固定肩锁关节,以减少韧带对喙突的牵拉有助于喙突复位,然后以空心拉力螺钉固定喙突骨折。
肩锁关节脱位是肩部常见损伤,越来越多的研究支持对喙锁韧带进行重建,并且临床上重建方法有多种。喙锁韧带由椎状韧带及斜方韧带构成,是限制锁骨向上及向后移位的重要韧带结构。椎状韧带及斜方韧带具有不同的功能,重建喙锁韧带时为达到良好效果需将两条韧带分别重建,有利于维持关节稳定性和恢复活动度。笔者在术中见位于喙锁韧带内侧部分的椎状韧带断裂,斜方韧带基本完整,用1枚直径3.0mm带线锚钉缝合固定喙锁韧带撕裂部分。
原始出处:
邓介超,丛云海,姜海军,杨波,王立超,史宗新.肩锁关节脱位合并喙突骨折及喙锁韧带部分断裂1例并文献复习[J].中国骨与关节损伤杂志,2019,34(07):778-779.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#关节脱位#
35
#部分断裂#
42
#肩锁关节#
33
#韧带#
40
#脱位#
46