Front Oncol:早期子宫内膜透明细胞癌患者行系统淋巴结切除术可改善患者预后
2022-03-29 yd2015 网络
研究表明,早期子宫内膜透明细胞癌患者行系统淋巴结切除术比未行系统淋巴结切除术的患者有更好的长期生存。
系统淋巴结切除术对子宫内膜癌的生存价值尚不明确且有争议。近期,国内团队开展了相关研究,目的是评估盆腔和腹主动脉旁联合淋巴结切除术对早期子宫内膜透明细胞癌患者的长期生存影响。相关结果发表在Frontiers in Oncology杂志上。
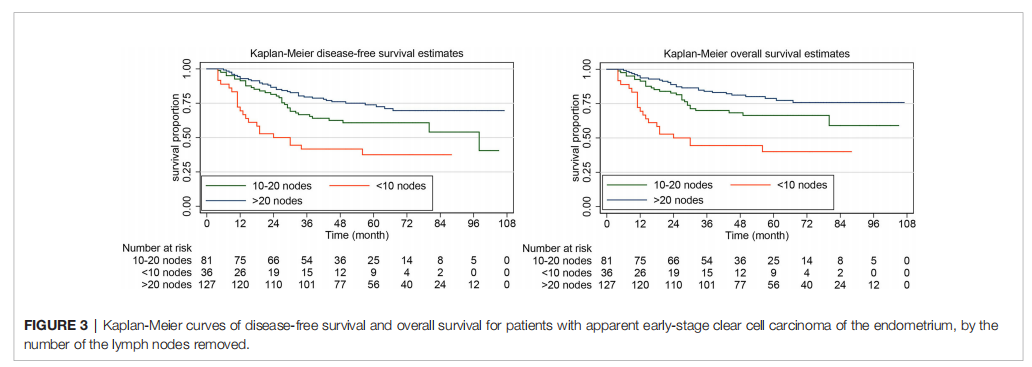
研究纳入三家中国教学医院2012 - 2017年早期子宫内膜透明细胞癌并进行手术分期的患者。进行和未进行系统淋巴结切除术的患者,比较两组的临床病理特征。通过Kaplan-Meier曲线和log-rank检验评估无病生存期(DFS)和总生存期(OS)。采用Cox比例风险模型来控制混杂因素。
244例患者进行了系统淋巴结切除术,89例未进行淋巴结清扫。两组间的人口统计和基线数据具有类似。
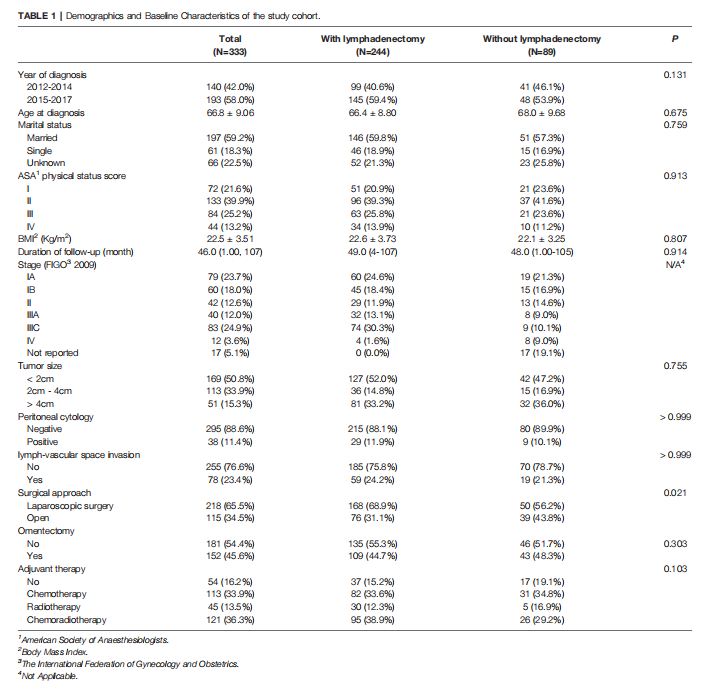
两组的2 cm及以上肿瘤大小比例(48.0%、52.9%,P=0.755)、LVSI(24.2%、21.3%,P>0.999),腹膜细胞学阳性(11.9%和10.1%,P>0.999)。在手术分期方式上,系统淋巴结清扫组腹腔镜手术率为68.9%,淋巴结保留组腹腔镜手术率为56.2%。在整个队列研究中,超过一半的患者(54.4%)行网膜切除术,40.5%的初始为早期病例的患者术后被归类为晚期(FIGO III期或IV期)。两组术后辅助治疗的比例相似,放化疗(36.3%)是最常见的辅助治疗方式,其次是化疗(33.9%)。
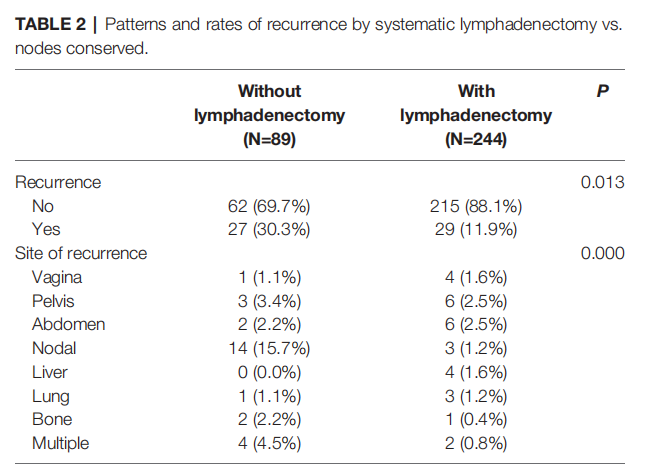
在未行系统淋巴结切除术的患者中,最常见的复发是淋巴结复发(15.7%),其次是多部位复发(4.5%)。而在接受全身淋巴结切除术的患者中,最常见的复发部位是骨盆(2.5%)和腹部(2.5%)。两组患者的复发率(P=0.013)和复发类型(P=0.000)比较,差异均有统计学意义。
行系统淋巴结清扫的患者5年无病生存率为64.10%,未行淋巴结清扫的患者5年无病生存率为45.05%。行系统淋巴结切除术的患者比未行淋巴结切除术的患者有更好的无病生存期(HR, 0.54, 95%CI,0.38 -0.76, P = 0.000)。
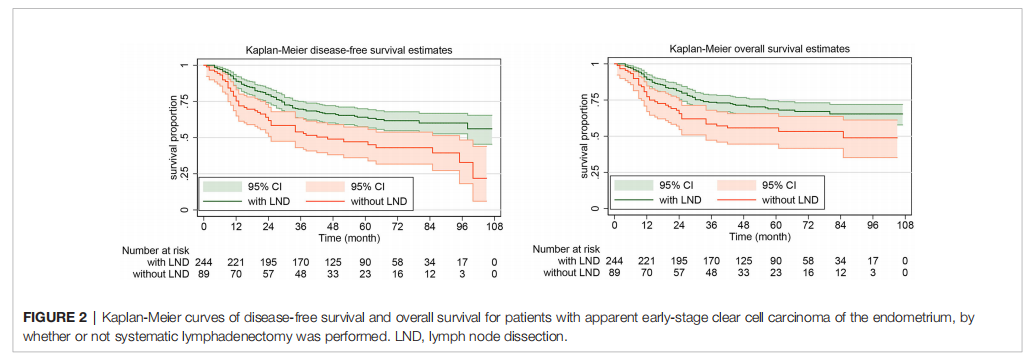
淋巴结切除术组的5年总生存率为68.87%(95% CI, 62.33%-74.51%),未行系统淋巴结切除术的患者的5年总生存率为53.33% 53.33% (95% CI, 41.63%-63.69%)。行系统淋巴结切除术的患者比未行淋巴结切除术的患者有更好的总生存期(HR, 0.58. 95% CI, 0.39-0.85. P=0.005)。
在接受系统淋巴结切除术的患者中,根据切除的淋巴结数目的亚分类进行生存分析。与切除少于10个区域淋巴结的患者相比,切除10 ~ 20个或20个以上区域淋巴结的患者的DFS和OS更好。
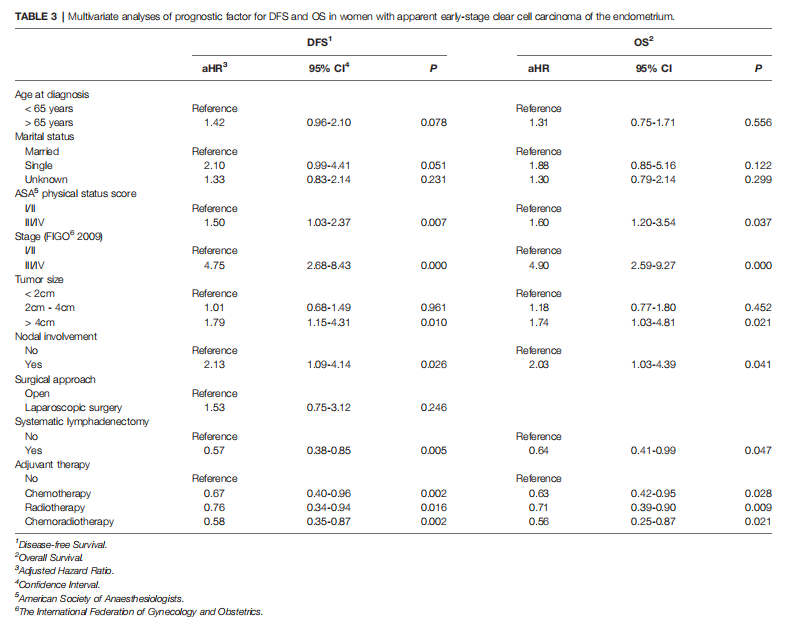
在对相关变量进行调整分析后,系统淋巴结切除术仍与早期子宫内膜透明细胞癌患者改善的DFS(aHR, 0.57,95%CI 0.39-0.85,P=0.005)和OS (aHR, 0.64,95%CI,0.41-0.99,P=0.047)独立相关。
综上,研究表明,早期子宫内膜透明细胞癌患者行系统淋巴结切除术比未行系统淋巴结切除术的患者有更好的长期生存。
原始出处:
Tian Y, Ran L, Liu Y, Xu Y, Shen J, Mi G-s and Ke F-m (2022) Systematic Lymphadenectomy and Oncological Outcomes of Women With Apparent Early-Stage Clear Cell Carcinoma of the Endometrium: A Multi-Institutional Cohort Study. Front. Oncol. 12:800957. doi: 10.3389/fonc.2022.800957.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#内膜#
44
#细胞癌#
59
#切除术#
35
#Oncol#
31
#透明细胞癌#
29
#患者预后#
29
#淋巴结#
53