NEJM:血流储备分数引导的PCI与冠状动脉搭桥手术的比较分析
2022-01-13 MedSci原创 MedSci原创
在三支冠状动脉疾病患者中,在1年时死亡、心肌梗死、卒中或重复血运重建的复合发生率方面,未发现FFR引导的PCI不劣于CABG。
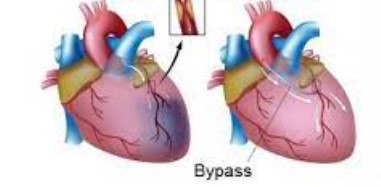
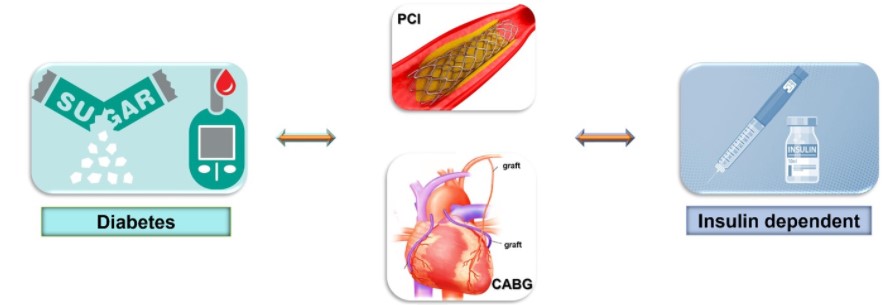
已有研究发现三支冠状动脉疾病患者的冠状动脉旁路移植术(CABG)比经皮冠状动脉介入治疗(PCI)有更好的结局,但以血流储备分数(FFR)指标为指导的PCI效果如何一直尚未明确。

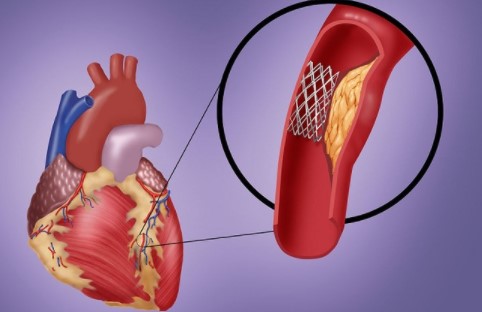
近日,顶级医学期刊NEJM上发表了一篇研究文章,在这项多中心、国际、非劣效性试验中,三支冠状动脉疾病患者被随机分配接受CABG或FFR引导的PCI,并使用当前一代佐他莫司洗脱支架。
该研究的主要终点是在1年内发生主要不良心脑血管事件,定义为全因死亡、心肌梗死、卒中或重复血运重建。FFR引导的PCI与CABG的非劣效性被预先设定为风险比的95%置信区间的上限小于1.65。次要终点包括死亡、心肌梗死或卒中的复合终点;研究人员还评估了其安全性。
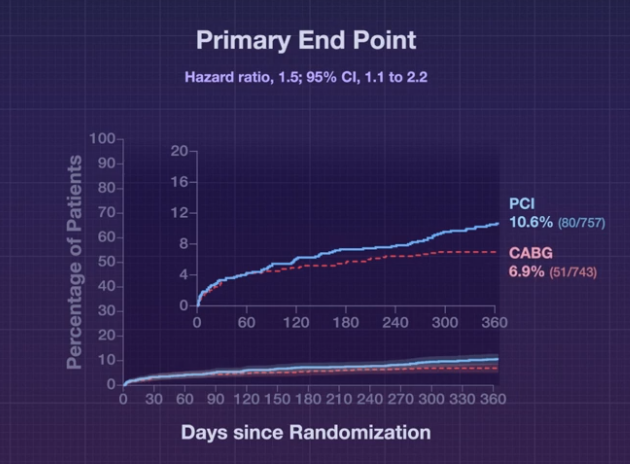
该研究共有1500名患者在48个中心接受了随机分组。接受PCI的患者平均植入了3.7±1.9个支架,接受CABG的患者接受了3.4±1.0处远端吻合。该研究的主要终点在随机分配接受FFR引导的PCI的患者中的1年发生率为10.6%,在分配接受CABG的患者中为6.9%(风险比为1.5;95%置信区间[CI]为1.1至2.2),FFR引导的PCI的结局非劣效性不一致(非劣效性P=0.35)。FFR引导的PCI组的死亡、心肌梗死或卒中发生率为7.3%,CABG组为5.2%(风险比为1.4;95%CI为0.9至2.1)。CABG组大出血、心律失常和急性肾损伤的发生率高于FFR引导的PCI组。
由此可见,在三支冠状动脉疾病患者中,在1年时死亡、心肌梗死、卒中或重复血运重建的复合发生率方面,未发现FFR引导的PCI不劣于CABG。
原始出处:
William F. Fearon,et al.Fractional Flow Reserve–Guided PCI as Compared with Coronary Bypass Surgery.NEJM.2021.https://www.nejm.org/doi/full/10.1056/NEJMoa2112299
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#搭桥#
38
#比较分析#
44
#PCI##冠心病#
117
#搭桥手术#
39
不错啊
44
11
47