胸闷气短别以为只是左心疾病 小心漏诊
2018-02-28 熊长明 肺血管病
例1 患者,男,67岁。因发作性胸闷8年入院,既往有糖尿病和高血压史。入院后行冠状动脉造影提示冠状动脉三支病变。遂行冠状动脉旁路移植术,术后1周开始间断发热,体温波动在37.5~38.5℃,应用多种抗菌素后仍然低热,并伴胸闷、气短,活动后加重。
例1 患者,男,67岁。因发作性胸闷8年入院,既往有糖尿病和高血压史。入院后行冠状动脉造影提示冠状动脉三支病变。遂行冠状动脉旁路移植术,术后1周开始间断发热,体温波动在37.5~38.5℃,应用多种抗菌素后仍然低热,并伴胸闷、气短,活动后加重。
查体:BP 110/70mmHg,左下肺呼吸音减弱,未闻及干湿性啰音,HR 86次/分,律齐,各瓣膜听诊区未闻及杂音,双下肢无水肿。动脉血气分析:pH 7.50,PO2 59.7mmHg,PCO2 29.8mmHg,HCO3-23.2mmol/L。D-二聚体10.29μg/ml。
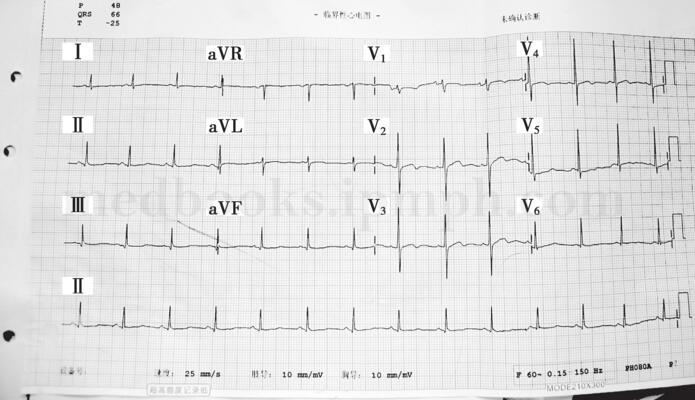
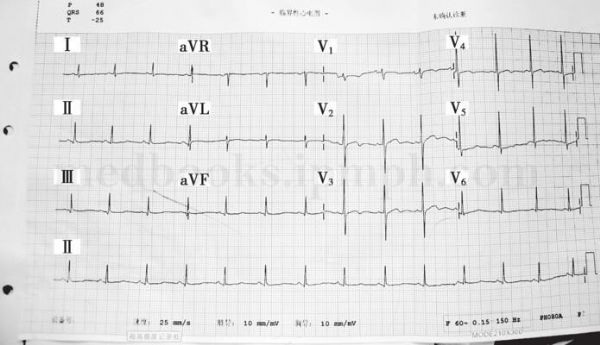
心电图(图28-1):窦性心律,ST-T改变。X线胸片(图28-2):两肺纹理重,左心室偏大,双侧少量胸腔积液。超声心动图:左心房35mm,左心室舒张末内径53mm,右心房、室不大,左心室射血分数 58%,下后壁运动相对减弱,余室壁运动正常,各瓣膜形态、结构、启闭运动未见明显异常。
首先考虑患者术后心功能不全,给予扩张冠脉、利尿等治疗后,症状无明显缓解。结合患者存在明显低氧血症、D-二聚体明显升高,有过手术和卧床病史,高度怀疑肺栓塞,行肺血管增强CT检查(图28-3),提示双肺多发性肺栓塞,双侧胸腔积液,立即给予低分子量肝素抗凝治疗,数天后患者症状明显缓解,体温恢复正常。
图28-1 心电图:窦性心律,ST-T改变
图28-2 X线胸片:两肺纹理重,左心室偏大,双侧少量胸腔积液
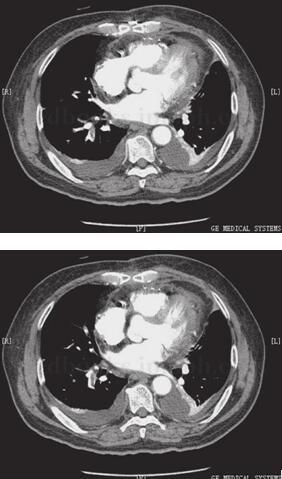
图28-3 肺血管增强CT检查:双肺多发性肺栓塞,双侧胸腔积液
例2 患者,男,59岁,因活动后胸闷、气短2年,右下肢水肿1个月入院,既往体健。2年前因活动后气短、乏力,外院行超声心动图检查诊断扩张型心肌病,给予对症治疗后症状好转,1个月前患者出现右下肢水肿,胸闷、气短症状较前有所加重,当地医院按心功能不全加重处理,右下肢水肿无明显消退。
入院后查体:BP 120/85mmHg,双肺呼吸音清晰,未闻及干湿性啰音,HR 70次/分,律齐,心尖部闻及2/6级收缩期吹风样杂音,右下肢水肿。动脉血气分析:pH 7.45,PO2 88.3mmHg,PCO2 40.3mmHg,HCO3-27.5mmol/L。D-二聚体3.59μg/ml。
胸片:两肺纹理重,全心扩大,心胸比0.7。心电图:心房颤动,ST-T改变。超声心动图:左心房50mm,左心室舒张末内径80mm,右心室37mm,左心室射血分数 30%,全心扩大,以左心室显著,室壁厚度正常,收缩幅度弥漫性减弱,估测肺动脉高收缩压50mmHg,二尖瓣瓣环扩大,瓣膜关闭欠佳,三尖瓣少量反流。
入院后考虑到患者按心功能不全加重处理后症状改善不明显,且仅有右下肢水肿,因此首先怀疑右下肢深静脉血栓形成,即行下肢多普勒超声检查提示右下肢深静脉血栓形成,同时肺血管增强CT提示多发性肺栓塞。立即在治疗扩张型心肌病基础上给予低分子量肝素和华法林抗凝治疗,1周后症状缓解、右下肢水肿明显消退。
【讨论】
左心疾病伴发肺栓塞出现的胸闷、气短等症状,一般首先想到左心疾病本身的问题,很少会考虑发生肺栓塞。第一例患者为老年男性,冠状动脉旁路移植术后出现胸闷、气短,间断发热,临床医师首先考虑患者术后心功能不全及感染,但患者的术后超声心动图检查提示心脏收缩功能基本正常,是否为舒张功能不全?即使为后者,一般经过利尿治疗症状应该很快好转,但该患者经过扩张冠脉和利尿治疗后症状没有缓解,笔者在查房时还发现患者即使在床旁小便即感到明显气短,但没有平卧后咳嗽和气短加重等不适,亦无胸痛,与超声心动图检查结果明显不符,且心电图与手术前无明显变化。立即查动脉血气和D-二聚体,提示明显低氧血症和D-二聚体水平升高。结合患者手术和卧床史,高度怀疑肺栓塞,肺血管增强CT检查随即证实为多发性肺栓塞,随后的抗凝治疗使患者症状明显缓解,体温也恢复正常,因此患者术后间断低热很可能为血栓吸收热。第二例患者为扩张型心肌病患者,出现胸闷、气短症状加重和下肢水肿很容易想到左心疾病的加重,但医师忽视的问题是心力衰竭的加重一般表现为双下肢水肿,而该患者是单侧下肢水肿,不好用心功能恶化来解释。单侧下肢水肿首先考虑的下肢深静脉血栓形成,患者D-二聚体明显升高,超声心动图提示肺动脉高压,临床上应高度疑诊肺栓塞,肺血管增强CT提示多发性肺栓塞。该患者在治疗扩张型心肌病基础上抗凝治疗取得明显效果。
结合上述2例病例分析,笔者认为左心疾病合并肺栓塞具有以下几个特点:①左心疾病伴有心功能不全时或手术后患者卧床少动,容易形成静脉血栓。②左心疾病合并肺栓塞的临床症状不易与左心疾病本身加重相鉴别。③由于左心疾病患者多伴有左心扩大和(或)肥厚,心脏除极电势总是左心室占优势。因此心电图很少表现为右心扩张和右心负荷加重的特征性表现,如SⅠQⅢTⅢ型、QRS电轴右偏、右束支传导阻滞等。④左心疾病患者的超声心动图多表现为左心房室扩大、室壁运动减弱、瓣膜关闭异常等,有些左心疾病本身可以合并右心扩大和(或)轻中度的肺动脉高压,当左心疾病合并肺栓塞时超声心动图的表现仍然以左心疾病的表现为主,右心系统的表现并不明显。以上特点也是造成左心疾病合并肺栓塞容易漏诊的主要原因。
笔者以为临床医师如果注意以下几点将有助于减少左心疾病合并肺栓塞的漏诊:①提高肺栓塞诊断意识;②当临床表现不能用左心疾病解释时,应把肺栓塞作为鉴别诊断的疾病之一;③不能解释的低氧血症;④重视D-二聚体的检测。D-二聚体是纤溶酶溶解的交联纤维蛋白的产物,只要体内存在活化的血栓形成及纤维蛋白溶解活动,D-二聚体就会升高,如心肌梗死、脑梗死、肺栓塞、静脉血栓形成、手术、肿瘤、弥散性血管内凝血、感染及组织坏死等均可导致D-二聚体升高。由于D-二聚体对急性肺栓塞诊断的敏感性高达92%~98%,而特异性仅为40%~43%,因此对急性肺栓塞有较大的排除诊断价值,若其含量低于500μg/L,可基本排除急性肺栓塞。⑤提高深静脉血栓形成(DVT)的诊断意识。临床医师不要忽视对患者下肢静脉疾病的问诊和查体,仔细询问DVT的易患因素,既往静脉血栓病史、下肢疼痛和肿胀症状等,检查下肢皮肤颜色、下肢周径、浅表静脉曲张等情况。⑥少数左心疾病患者的心电图和(或)超声心动图的表现不能用左心疾病本身来解释。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习了.谢谢作者分享!
61
学习了.谢谢作者分享!
62
学习了谢谢分享!!
62
#胸闷#
36
#漏诊#
28
#气短#
44
学习谢谢分享
51