Nat Commun:前列腺癌中雄激素受体信号途径和PARP通路之间的合成致死作用
2017-09-02 AlexYang MedSci原创
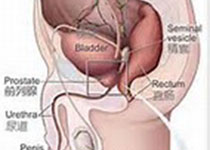
最近,来自英国剑桥大学癌症研究中心的一项研究表明,前列腺癌中雄激素受体信号途径和PARP通路之间具有合成致死作用。越来越多的数据阐释了同源重组(HR)在去势难治性前列腺癌中的缺陷,致使这些肿瘤对PARP抑制作用表现为敏感。最近,研究人员阐明了雄激素受体(AR)来维持HR基因的表达和在前列腺癌中HR活性的直接需求。研究发现,在雄激素阻断治疗(ADT)后,PARP调控的修复通路在前列腺癌中表达上调。更
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
17
#COMMUN#
24
#雄激素受体#
23
#信号途径#
29
#PARP#
0
学习了.涨知识
50