Nat Commun:潜在新疗法使用PHD抑制剂缓解月经过多
2018-01-24 Nature自然科研 Nature自然科研
本周《自然-通讯》发表的一项研究Hypoxia and hypoxia inducible factor-1α are required for normal endometrial repair during menstruation借助小鼠模型,展示了一种或可代替手术和激素疗法的月经过多疗法。每5名女性,至少有1名在一生当中的某个时刻会经历月经过多,她们或是接受手术或是采用激素疗法,前者常常会
本周《自然-通讯》发表的一项研究Hypoxia and hypoxia inducible factor-1α are required for normal endometrial repair during menstruation借助小鼠模型,展示了一种或可代替手术和激素疗法的月经过多疗法。每5名女性,至少有1名在一生当中的某个时刻会经历月经过多,她们或是接受手术或是采用激素疗法,前者常常会导致不孕,后者则往往会产生各种副作用。因此,有必要开展更多的研究来找到可代替它们的治疗方法。
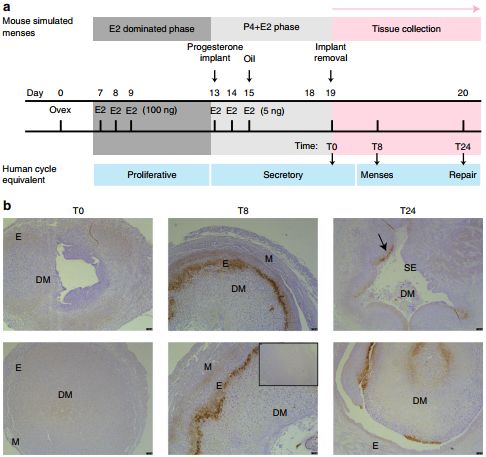
月经小鼠模型揭示了月经期的生理低氧状态。DM 蜕膜块,E 子宫内膜,M 子宫肌层,SE表面上皮。
没有怀孕的女性子宫内膜脱落,引起出血,形成月经。子宫内膜成功修复后,则停止出血。不少女性在经期会出现剧痛和出血过多的情况,面临着严重贫血风险。
英国爱丁堡大学的Jackie Maybin、Hilary Critchley和同事表明,子宫内膜需要低氧才能成功修复。他们利用一种名为PHD抑制剂的药品治疗月经小鼠模型,表明PHD抑制剂可以“诱骗”子宫认为氧含量低,促进子宫内膜修复。他们的实验表明,PHD抑制剂或可用于加速女性子宫内膜修复,从而减少经期出血和其它相关症状,不过还需要更进一步的研究来验证该方法在人体内的效果。

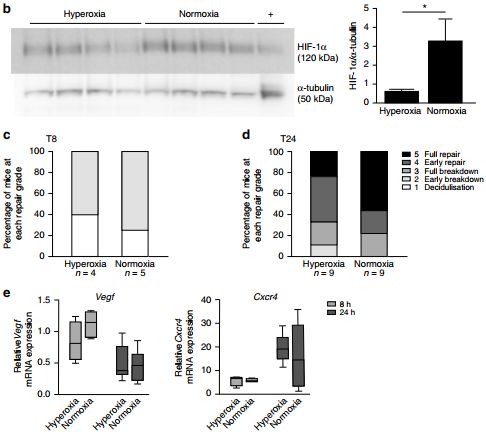
非缺氧状态的月经减少了子宫内膜的HIF-1α水平并延缓了内膜修复。
原始出处:
Jacqueline A. Maybin, Alison A. Murray, Philippa T. K. Saunders, et al.Hypoxia and hypoxia inducible factor-1α are required for normal endometrial repair during menstruation.Nature Communications 9, Article number: 295 (2018) doi:10.1038/s41467-017-02375-6.Published online:23 January 2018
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#COMMUN#
32
#PhD#
35
#Nat#
21
#抑制剂#
23
#月经#
25
#新疗法#
25