Lancet:无心血管风险因素的ST抬高型心肌梗死患者的全因死亡率显著高于有风险因素的患者!
2021-03-10 MedSci原创 MedSci原创
无心血管风险因素的个体发生ST抬高型心肌梗死后的死亡率竟然高于有风险因素的患者!!
对于心血管疾病,针对标准可修改的心血管危险因素(SMuRF;高血压、糖尿病、高脂血症和吸烟)的预防策略至关重要。
然而,在不存在SMuRF的情况下,心肌梗死仍不罕见。无SMuRF的个体发生心肌梗死的预后仍未有很好的评估。
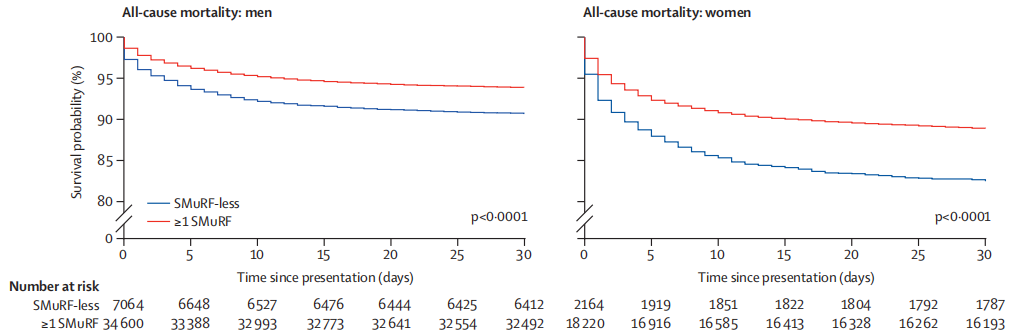
本研究采用瑞典心肌梗死注册表SWEDEHEART的数据回顾性地分析了首次出现ST抬高型心肌梗死(STEMI)的成年(≥18岁)患者,对比了有无SMuRF的患者的临床特征和预后。排除有冠状动脉疾病病史的患者。主要终点是STEMI发生后30天内的全因死亡率。
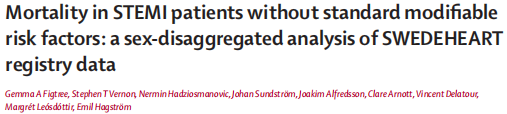
主要终点的风险比
2005年1月1日-2018年5月25日,共62048位STEMI患者被纳入分析,其中9228位(14.9)无SMuRF情况。有无SMuRF情况的患者的平均年龄相近(68 vs 69岁)。无SMuRF情况的患者经皮冠状动脉介入治疗的概率与具有至少一种可改变的危险因素的患者的相似,但在出院时接受他汀类药物、血管紧张素转换酶抑制剂(ACEI)或血管紧张素受体阻滞剂(ARB)或β受体阻滞剂治疗的患者的经皮冠状动脉介入治疗可能性显著降低。
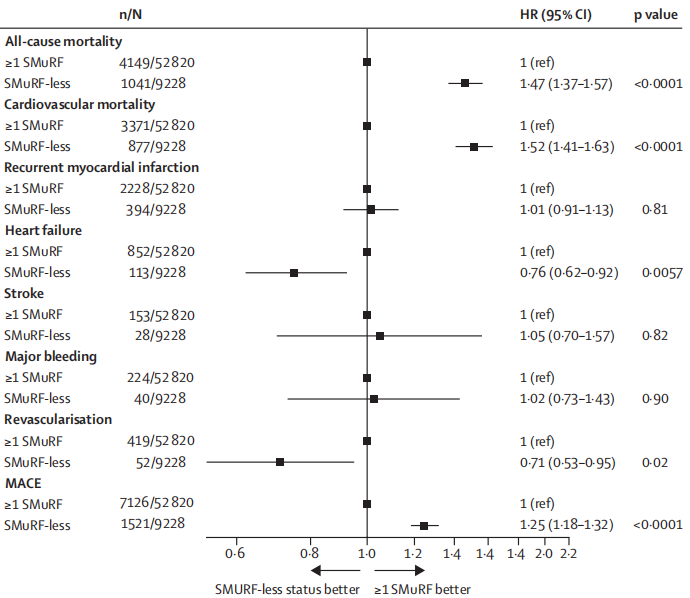
30天内的全因死亡率
在STEMI发生后30天时,无SMuRF情况的患者的全因死亡率明显更高(风险比 1.47, 95% CI 1.37-1.57, p<0.0001)。无SMuRF情况的女性患者的30天死亡率最高(17.6%),其次是有SMuRF情况的女性患者(11.1%)、无SMuRF情况的男性患者(9.3%)和有SMuRF情况的男性患者(6.1%)。
不同性别患者的全因死亡率
经年龄、性别、左心室射血分数、肌酐和血压校正后,无SMuRF情况的患者的30天全因死亡风险增加仍具有显著意义,但加入出院时的处方药物(ACEI或ARB、β受体阻滞剂或他汀类药物)后则减弱。
此外,与有一项或多项SMuRF情况的患者相比,无SMuRF情况的患者的院内全因死亡率也明显更高(9.6% vs 6.5%,p<0.0001)。无SMuRF情况的患者的30天内心肌梗死和心衰的发生率较低。在长期随访过程中,无SMuRF情况的患者的全因死亡率持续保持增长,在男性患者中超过了8年,在女性患者中持续到12年随访终点。
与至少有一项SMuRF情况的患者相比,在没有SMuRF的情况下发生STEMI的个体的全因死亡风险显著增加,这在女性中尤为明显。
原始出处:
Gemma A Figtree, et al. Mortality in STEMI patients without standard modifiable risk factors: a sex-disaggregated analysis of SWEDEHEART registry data. The Lancet. March 09, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#心肌梗死#
103
#ST抬高型心肌梗死#
32
#血管风险#
38
#Lancet#
23
#全因死亡率#
34
顶刊就是不一样,质量很高,内容精彩!学到很多
38
好文章!
63
收藏
75