女性,41岁。咳嗽半月,时有胸闷,两年前外伤史。
X线胸片:右中下肺密度增高,中上肺见多个液平,右膈抬高,膈面及肋膈角消失,纵隔左移,右侧多发肋骨骨折(图1A)。

图1A 纵隔左移,右侧多发肋骨骨折CT平扫:右侧胸廓明显扩大,纵隔影明显受压推移,右胸外侧见肠管影及网膜影,肠管扩张并气液平,上至肺尖,右肺受压不张,部分肺组织疝入右侧胸腔(图1B,1C)。
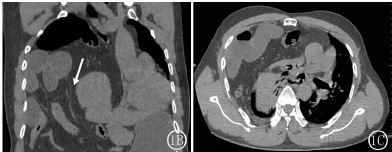
图1B,1C 右肺受压不张,部分肺组织疝入右侧胸腔右膈肌断裂回缩内移增厚,呈条带状软组织密度似“飘带征”;腹腔肠管、网膜及部分肝脏通过膈肌裂口疝入胸腔呈“领口征”(图2)。

图2 右膈肌断裂回缩增厚,呈条带状软组织密度影由于膈肌破裂位于右外侧,肠影及网膜影聚集肝右外侧,肝脏明显受压推移,肝下缘肠管扩张积液伴气液平,肠壁增厚。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#创伤性#
29
#创伤#
25
#陈旧性#
40
#疝#
39