J Cell Mol Med:circRFWD2和circINO80可促进人脂肪源性干细胞的成骨过程
2020-10-03 网络 网络
骨缺损给全世界造成了沉重的社会和经济负担。Nel-like molecule, type 1 (NELL-1)可以促进成骨和骨缺损的修复,但具体机制尚待阐明。循环RNAs(circRNAs)已被发现在
骨缺损给全世界造成了沉重的社会和经济负担。Nel-like molecule, type 1 (NELL-1)可以促进成骨和骨缺损的修复,但具体机制尚待阐明。循环RNAs(circRNAs)已被发现在组织发育中发挥关键作用,并作为各种疾病的生物标志物。然而,circRNAs的表达模式及其在重组NELL-1诱导的人脂肪源性干细胞(hASCs)成骨过程中发挥的作用仍不清楚。

本研究中,我们对重组NELL-1诱导的成骨分化过程中circRNA的表达谱进行了RNA测序研究,鉴定出两个关键的circRNA,即circRFWD2和circINO80。研究证实这两个circRNA在重组NELL-1诱导的成骨过程中上调,敲除这两个circRNA会影响NELL-1对成骨的积极作用。CircRFWD2和circINO80可以与hsa-miR-6817-5p相互作用,从而抑制成骨作用。沉默hsa-miR-6817-5p可以部分逆转si-circRFWD2和si-circINO80对成骨的负面影响。
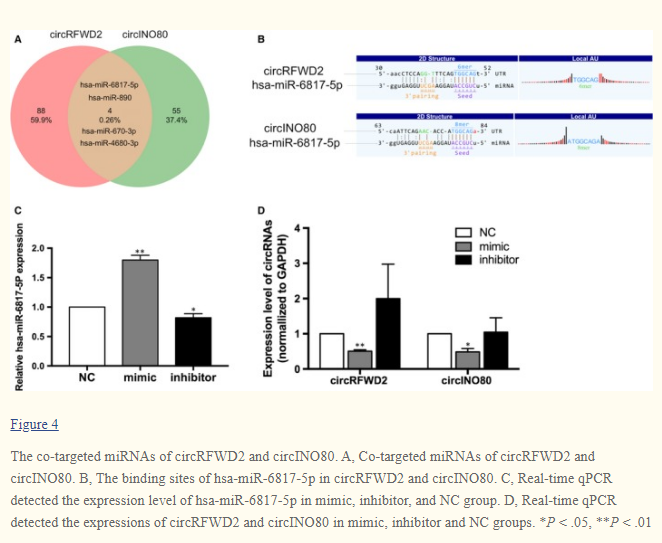
因此,circRFWD2和circINO80可以调节hsa-miR-6817-5p的表达,影响重组NELL-1诱导的hASCs成骨分化。这为更好地了解NELL-1对hASCs成骨分化的影响打开了一扇新的窗口,为高效安全地进行骨再生提供了潜在的分子靶点和新方法。
原始出处:
Xinqi Huang, Xiao Cen, et al., The roles of circRFWD2 and circINO80 during NELL-1-induced osteogenesis. J Cell Mol Med. 2019 Dec;23(12):8432-8441. doi: 10.1111/jcmm.14726.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CEL#
0
#CIN#
28
#CRF#
37
#Cell#
28
干细胞是热点,但是进入临床仍然需要时间和临床疗效验证哦
47
#成骨#
56
#Med#
23