Nature子刊:利用pNaKtide降低氧化应激或有助治疗尿毒症心肌病
2016-10-06 佚名 生物谷
在一项新的研究中,来自美国马歇尔大学、托雷多大学和纽约医学院的研究人员针对最近发现的Na/K泵(sodium-potassium pump)的信号转导功能进一步开展研究,鉴定出这一发现的一项重要的应用,从而可能潜在地导致人们开发出治疗肾脏疾病患者的新疗法。相关研究结果于2016年10月4日在线发表在自然出版集团旗下的Scientific Reports期刊上,论文标题为“Attenuation o
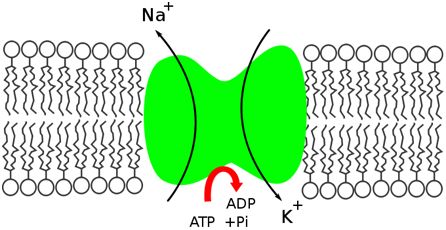
这项研究的发现提示着导入肽pNaKtide降低氧化应激(oxidant stress)能够缓解实验性尿毒症心肌病(uremic cardiomyopathy),即一种几乎总是伴随着晚期肾功能衰竭的心脏病。尽管在美国,需要透析或器官移植的晚期肾功能衰竭仅影响每1***中的大约1到2人,但是较为温和的慢性肾脏疾病是非常常见的(占成年人人群的25%),而且也似乎与增加的心血管疾病发病率和死亡率相关联。
论文通信作者、马歇尔大学琼-爱德华兹医学院(Joan C. Edwards School of Medicine)主任Joseph I. Shapiro博士说,“我们的数据明确地表明这种肽显著地阻止和逆转小鼠体内的实验性尿毒症心肌病产生。这些发现提示着我们可能为之前无法治疗的疾病开发出有效的疗法。我想强调一下,当前的这项研究明确地确定了Zijian Xie博士在二十世纪九十年代晚期发现的这种Na/K泵的信号转导功能是一种重要的治疗靶标。”
Zijian Xie博士是马歇尔大学交叉学科研究所主任和马歇尔大学琼-爱德华兹医学院生物医学科学教授。
Xie说,“作为一名基础研究科学家,我特别高兴地看到我们针对这种Na/K泵的信号转导功能的发现可能真正地影响人类健康和临床医学。毋庸讳言,针对这种新的治疗靶标开发一种有效的药物仍然有好长的路要走。然而,我们对这种新的机会仍然感到非常激动人心。”
Jiang Liu, Jiang Tian, Muhammad Chaudhry, Kyle Maxwell, Yanling Yan, Xiaoliang Wang, Preeya T. Shah, Asad A. Khawaja, Rebecca Martin, Tylor J. Robinette, Adee El-Hamdani, Michael W. Dodrill, Komal Sodhi, Christopher A. Drummond, Steven T. Haller, David J. Kennedy, Nader G. Abraham, Zijian Xie & Joseph I. Shapiro.Attenuation of Na/K-ATPase Mediated Oxidant Amplification with pNaKtide Ameliorates Experimental Uremic Cardiomyopathy.Scientific Reports.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
26
#Akt#
27
继续关注!
38
谢谢分享!
29
#尿毒症#
25
#应激#
16
#肌病#
17