JACC:DTBT时间越短,心梗患者预后越好!
2015-12-29 QQduph 译 MedSci原创
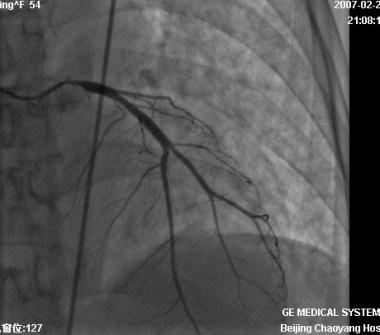
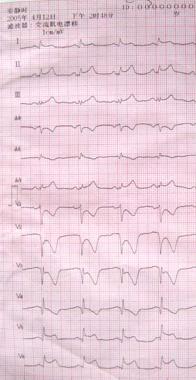
DTBT时间是患者在院外出现心脏病发作至抵达急诊室经皮冠状动脉介入并恢复血液流动之间的时间。 根据美国心脏协会的描述了,SI段抬高型心肌梗死(STEMI)是一种严重的心脏病,并导致心脏血流受阻而使心脏大面积受损。美国心脏病协会建议(ACC),STEMI患者应该在入院90分钟内行经皮冠状动脉介入治疗。 约90%的患者经皮冠状动脉介入术后,心脏表面血流恢复,但约1/3的患者心肌血流量未恢复。这项研究的
DTBT时间是指患者在院外出现心脏病发作至抵达急诊室经皮冠状动脉介入并恢复血液流动之间的时间。
根据美国心脏协会的描述,ST段抬高型心肌梗死(STEMI)是一种严重的心脏病,并导致心脏血流受阻而使心脏大面积受损。美国心脏病协会建议(ACC),STEMI患者应该在入院90分钟内行经皮冠状动脉介入治疗。
约90%的患者经皮冠状动脉介入术后,心脏表面血流量恢复,但约1/3的患者心肌血流量未恢复。
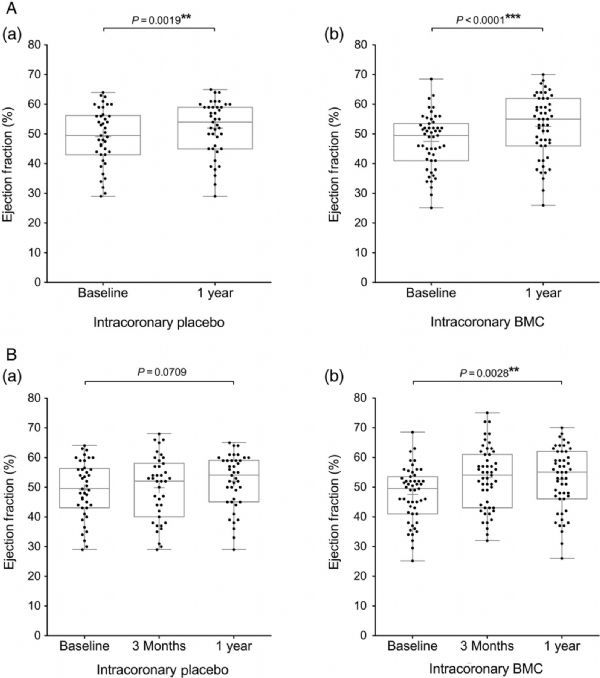
这项研究的研究人员比较了心脏病发作患者DTBT时间长短差异对民众心肌功能的影响。
研究人员回顾了HORIZONS-AMI研究中2056名心肌梗死后接受血管再造和支架的患者,他们比较了三个时间段患者的症状及治疗效果:小于2小时、2-4个小时、超过4小时。
结果表明,患者在出现心梗症状后2-4小时内或更久接受球囊成形术后心脏血流量恢复情况较患者再出现心梗症状后2小时内接受球囊成形术的患者好,且3年内死亡率更高。
Roxana Mehran博士认为,近年来研究显示,DTBT时间的减少并不会导致STEMI患者死亡率降低。这项研究强调了需要重新考虑球囊成形术工具的度量、最初医治及首次气囊使用时间及心肌缺血时间。
Michael A. Kutcher博士认为,DTBT时间是非常宝贵的,应该尽可能缩短,但是医生需要仔细评估患者心肌缺血的症状和体征或血流减少情况。且医务人员应该对患者进行详细的健康宣教。
原始出处:
There is a need to recognize heart attack symptoms more quickly,MNT,29,Dec,2015
Abhiram Prasad et al.Effect of ischemia duration and door-to-balloon time on myocardial perfusion in ST-segment elevation myocardial infarction: an analysis from HORIZONS-AMI trial (Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction).JACC: Cardiovascular Interventions.28 Dec,2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JACC#
25
#心梗患者#
29
#患者预后#
37
了解了DTBT,
106
不错,
87
不错,
120
希望对临床有指导作用,
100
希望对临床有指导作用,
107
感谢分享,
90
值得学习
51