Thorax:无家可归人群中潜伏性结核病和血源性病毒感染的患病率较高!
2018-01-30 xing.T MedSci原创
由此可见,这项研究结果表明无家可归者中LTBI的患病率很高,而且相关的护理工作也很差。在这一群体中,对LTBI和丙型肝炎感染治疗以及乙肝疫苗接种存在很大的需求。
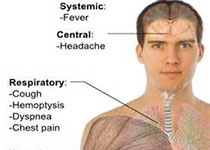
英国城市无家可归人群的活动性肺结核发病率很高,但潜伏性结核感染(LTBI)患病率较低。近日,胸部疾病领域权威杂志Thorax上发表了一篇研究文章,该研究旨在评估无家可归个人LTBI的患病率。
研究人员对伦敦的无家可归个人进行了一项横断面调查以及结局随访。该研究的主要结局为LTBI的患病率。该研究招募的时间为2011年5月至2013年6月。为了估计LTBI患病率为10%,95%可信区间在8%至13%之间,该研究需要500名参与者。
该研究中491/804(61.1%)的参与者同意进行筛查。LTBI的患病率为16.5%(81/491; 95%CI为13.2-19.8)。在英国出生的个体中,调整了年龄、无家可归时间和非法药物使用后,监禁史与LTBI风险增加有关(比值比为3.49; 95%CI为1.10-11.04; P=0.018)。过去乙肝感染的患病率为10.4%(51/489; 95%可信区间为7.7-13.1),59.5%(291/489; 95%CI为55.1-63.9)的个体无免疫力。目前丙型肝炎感染的患病率为10.4%(51/489; 95%CI为7.8-13.1)。
由此可见,这项研究结果表明无家可归者中LTBI的患病率很高,而且相关的护理工作也很差。在这一群体中,对LTBI和丙型肝炎感染治疗以及乙肝疫苗接种存在很大的需求。
原始出处:
Robert W Aldridge, et al. High prevalence of latent tuberculosis and bloodborne virus infection in a homeless population.Thorax. 2018.http://dx.doi.org/10.1136/thoraxjnl-2016-209579
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






学习了.谢谢分享
41
了解了解.继续关注
44
#患病率#
24
#结核#
20