Gastric Cancer:帕博利珠单抗(Pembrolizumab)vs 紫杉醇治疗既往治疗过PD-L1阳性胃或胃食管连接处癌的疗效:III期临床研究KEYNOTE‑061的2年更新结果
2021-09-11 yd2015 MedSci原创
该研究表明,随着PD-L1的表达增加,帕博利珠单抗较紫杉醇可改善胃或胃食管连接处癌的OS,并且不良反应较少。
KEYNOTE-061是一项随机、开放标签、3期临床试验,评估帕博利珠单抗(Pembrolizumab)vs 紫杉醇用于既往治疗过的晚期胃或胃食管连接处癌的疗效。在PD-L1 CPS ≥1的患者中(数据截止日期:2017年10月26日),与紫杉醇相比,帕博利珠单抗并没有显著改善患者的总生存期(OS)(HR=0.82; 95%CI 0.66-1.03;单侧P = 0.0421)或无进展生存期(PFS)( HR=1.27; 95% CI 1.03–1.57)。帕博利珠单抗治疗组的应答持续时间(DOR)明显长于紫杉醇组(中位数,18.0 vs 5.2个月),而且帕博利珠单抗比紫杉醇具有更好的安全性。近期,Gastric Cancer杂志更新了随访结果。

在数据截止时,366例PD-L1 CPS≥1患者死亡(帕博利珠单抗组为176/196[89.8%],紫杉醇组为190/199 [95.5%]); 帕博利珠单抗组的中位OS为9.1个月(95% CI 6.2-10.7),紫杉醇组的中位OS为8.3个月(95% CI 7.6-9.0)( HR= 0.81;95%CI 0.66-1.00)。随着随访时间的延长,与紫杉醇相比,帕博利珠单抗显示了改善OS的趋势。170例PD-L1 CPS≥5患者死亡(帕博利珠单抗组为84/95 [88.4%],紫杉醇组为86/91 [94.5%]); 帕博利珠单抗组的中位OS为10.4个月(95% CI 6.7–15.5),紫杉醇组的中位OS为8.3个月(95% CI 6.8–9.4)( HR= 0.72; 95% CI 0.53–0.99)。95例PD-L1 CPS≥10患者死亡(帕博利珠单抗组为44/53 [83.0%],紫杉醇组为51/55 [92.7%]); 帕博利珠单抗组的中位OS为10.4个月(95% CI 5.9–18.3),紫杉醇组的中位OS为8.0个月(95% CI 5.1–9.9) ( HR= 0.69; 95% CI 0.46–1.05)。
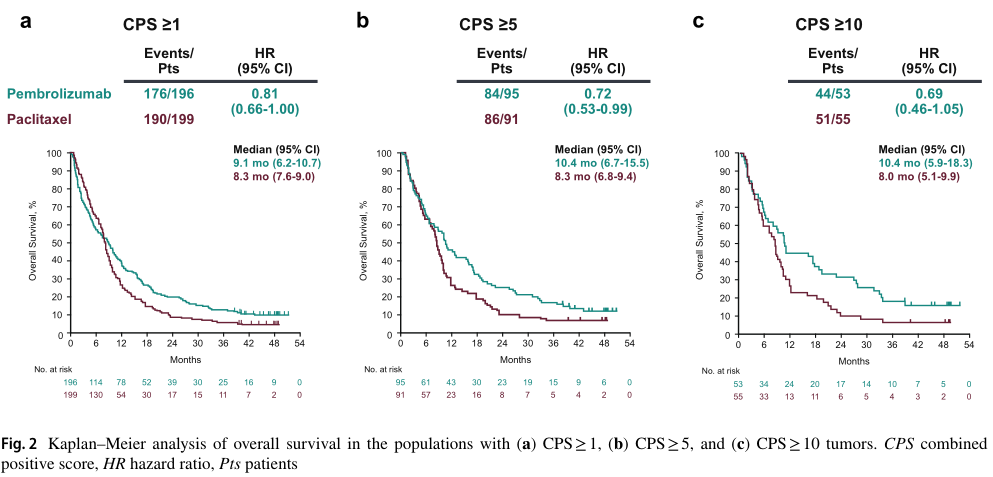
OS
PD-L1 CPS≥1和ECOG PS=0的患者中, 帕博利珠单抗组和紫杉醇组的中位OS分别为12.3个月(95% CI 9.7–15.9)和9.3个月(95% CI 8.3–10.5) ( HR= 0.69; 95%CI 0.50–0.95);PD-L1 CPS≥1和ECOG PS=1的患者中, 帕博利珠单抗组和紫杉醇组的中位OS分别为5.4个月(95% CI 3.7–7.7)和7.5个月(95% CI 5.3–8.4) ( HR= 0.98; 95% CI 0.74–1.31)。
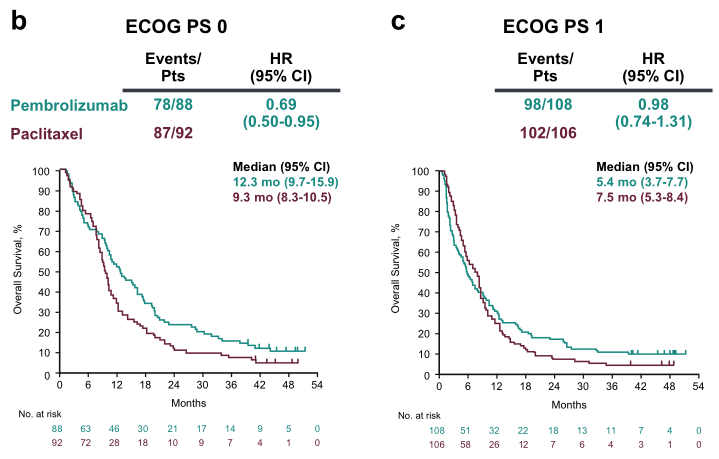
不同PS评分的OS比较
PD-L1 CPS≥1患者,帕博利珠单抗组和紫杉醇组的中位PFS分别为1.5 个月(95% CI 1.4–2.0)和4.1个月(95% CI 3.2–4.3) ( HR= 1.25; 95% CI 1.02–1.54)。PD-L1 CPS≥5患者,帕博利珠单抗组和紫杉醇组的中位PFS分别为1.6个月(95% CI 1.4–2.8)和4.0个月(95% CI 2.8–4.4) ( HR= 0.98; 95% CI 0.71–1.34)。PD-L1 CPS≥10患者,帕博利珠单抗组和紫杉醇组的中位PFS分别为2.7个月(95% CI 1.4–4.3)和4.0个月 (95% CI 2.7–4.4) ( HR= 0.79; 95% CI 0.51–1.21)。
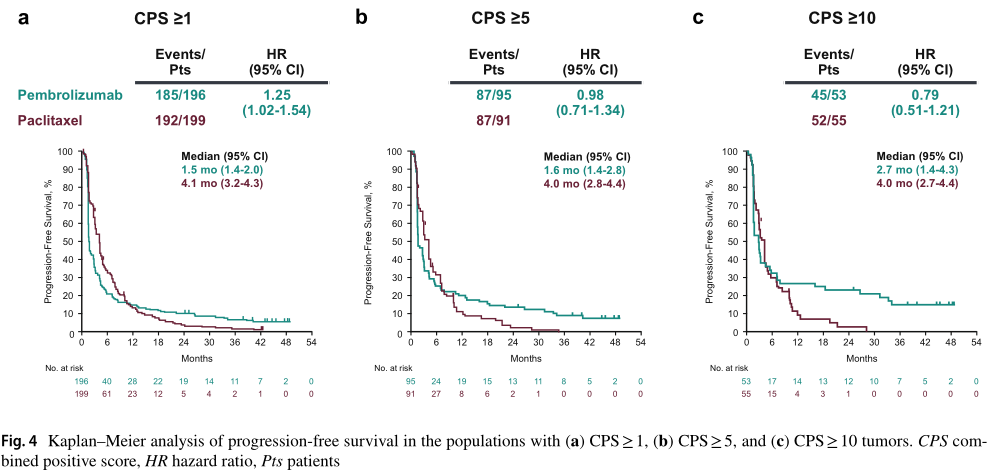
PFS
ORR(帕博利珠单抗vs紫杉醇)分别为16.3% vs 13.6% (CPS ≥1)、20.0% vs 14.3% (CPS ≥5)和24.5% vs 9.1% (CPS ≥10);中位DOR分别为19.1个月vs 5.2, 32.7个月vs 4.8个月, NR vs 6.9个月。

ORR
帕博利珠单抗组的治疗相关不良反应较紫杉醇组的少,分别为53%和84%。
综上,该研究表明,随着PD-L1的表达增加,帕博利珠单抗较紫杉醇可改善胃或胃食管连接处癌的OS,并且不良反应较少。
原始出处:
Fuchs CS, Özgüroğlu M, Bang YJ, et al. Pembrolizumab versus paclitaxel for previously treated PD-L1-positive advanced gastric or gastroesophageal junction cancer: 2-year update of the randomized phase 3 KEYNOTE-061 trial. Gastric Cancer. 2021 Sep 1. doi: 10.1007/s10120-021-01227-z. Epub ahead of print. PMID: 34468869.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#II期临床研究#
60
#帕博利珠#
50
#III#
51
#mAb#
37
#胃食管#
42
#KEYNOTE#
50
#I期临床#
40
#Pembro#
51
#III期临床研究#
42
#gastric#
28