先天性髋关节脱位的切开复位术
2016-01-06 MedSci MedSci原创
切开复位术 除少数先天性髋关节脱位因过去未经治疗,而成年后不可能复位者,其余先天性髋脱位病人的基本手术是切开复位术。手术年龄可达少年青春期,如为半脱位可延长至成年期或更晚。对病理改变不重、多数在4岁以内的幼儿,单纯切开复位即可使之完全治愈;但对病理改变重,尤其是髋臼改变大者,切开复位必须辅以相应的矫形手术才得痊愈。 切开复位术的目的是使股
切开复位术
除少数先天性髋关节脱位因过去未经治疗,而成年后不可能复位者,其余先天性髋脱位病人的基本手术是切开复位术。手术年龄可达少年青春期,如为半脱位可延长至成年期或更晚。对病理改变不重、多数在4岁以内的幼儿,单纯切开复位即可使之完全治愈;但对病理改变重,尤其是髋臼改变大者,切开复位必须辅以相应的矫形手术才得痊愈。
切开复位术的目的是使股骨头在髋臼内得到同心圆坐落,也即是恢复髋关节的解剖学位置,从而为病人能恢复正常功能创造条件。要达到这一目的,需要消除所有阻碍股骨头复位的因素,包括关节内、关节外因素,也包括骨性的和软组织性的因素。
[适应证]
1.4~5岁以内的病儿经手法复位失败者,或不适宜于非手术疗法的5~9岁病儿,均可行髋关节切开复位术。年龄大、病理改变重者需辅以其他手术。
2.髋臼、股骨头相称,但臼较浅,髋臼角在45°以内的病儿,可在切开复位的同时施行髋骨放置切骨术;如髋臼角大于45°,应施行髋臼成形术。
3.髋臼小而浅,不能容纳股骨头,应在切开复位的同时施行髋臼加盖术;年龄较大,股骨头脱位已不可能切开复位,假臼平浅,关节又很不稳定者,可考虑原地假臼加盖术,以改善功能。
4.股骨颈前倾角超过45°或颈干角在140°以上者(正常前倾角为15°,颈干角为120°~130°),应在髋关节切开复位的同时或二期手术行股骨旋转切骨术或内收切骨术。
5.成年先天性髋关节半脱位的病人;男性儿少年先天性髋关节脱位不适宜施行骨盆旋转切骨、髋臼成形或加盖术者,可旅行骨盆内移切骨术(chiari手术)。
6.15岁以上的病人不宜施行以上各种手术时,对严重畸形、关节不稳定、负重线不佳而引起髋关节或腰背部疼痛的病人,可考虑做改善负重线和稳定性手术(如股骨转子下切骨术或髋关节融合术等)。
[术前准备]
1.术前须常规行病肢牵引,使股骨头从髋臼的后上方回到髋臼水平,这一步骤十分重要。牵引可使挛缩的肌肉松弛,一方面可使手术复位容易成功,并可防止术后再脱位;另一方面可以减少股骨头复位后因受压而发生软骨面坏死和股骨头缺血性坏死的机会。年龄较小的、脱位不重的病儿可用皮牵引;年龄较大的应采用胫骨粗隆牵引。一般牵引2~3周即可使股骨头下降到髋臼平面,经X线摄片证实后,适当减轻重量,维持股骨头在该平面1~2周,即可施行手术。
2.若经过牵引,股骨头下降不明显,应检查是否由于股内收肌或臀肌挛缩紧张所致。有此情况者应作内收肌起点切断术或松解术,再继续牵引病肢,达到牵引要求为止。一般来讲,凡超过2~3岁者,均需切断可松解。
3.术前病例髋关节周围和下肢备皮3日。
4.术前要较准确地测定前倾角,髋外翻角,选定加盖部位,髋切骨部位,然后作好股骨或髋骨切骨后旋转角度、植骨块大小等的手术设计。
5.备血200~600ml。
[麻醉]
1.全麻。
2.基础麻醉加骶管麻醉或硬膜外麻醉。
[手术步骤、术中注意事项]
1.体位 平卧位,病侧臀部垫高,使臀部与手术台成30°角。
 |
 |
| ⑴前外侧皮肤切口,显露切开髂嵴 | ⑵骨膜下剥离,显露髂骨翼内侧面 |
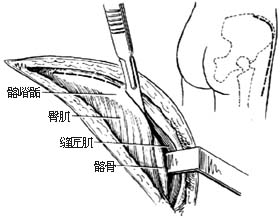
2.切口、显露 采用髋关节前外侧切口(见髋关节显露途径)。但此种病人多为儿童,髂嵴骨骺应注意保留,以免病儿骨盆发育障碍。显露髂嵴软骨后,先沿其中线纵行切开软骨[图1 ⑴]。再在骨骺线平面向两侧切至骨膜下,用骨膜剥离器把髂肌连带内半髂嵴软骨从髂骨翼内侧面作骨膜下推开[图1 ⑵],迅速用干纱布在骨膜下堵塞止血;再将外侧的阔筋膜张肌、臀中肌、臀小肌连带外半髂嵴软骨从髂骨翼外侧面作骨膜下推开[图1 ⑶],同样以干纱布迅速堵塞止血。用小拉钩把缝匠肌拉向内侧,于髂前下棘切断股直肌,将其向下翻开。此时,髂骨翼内、外侧面和髋关节均可充分显露。在髋臼的后上方可找到脱位的股骨头和随之向后上延伸、增厚的髋关节囊[图1 ⑷]。
 |
 |
| ⑶骨膜下剥离,显露髂骨翼外侧面 | ⑷延长髂腰肌,显露并切开葫芦形关节囊 |
3.清理关节、消除复位障碍 先沿髋臼的边缘1.5~2cm处弧形切开增厚的关节囊,检查关节囊有无狭窄变形。股骨头向髋臼后上方脱位,常使髂腰肌挛缩,成为一条索带,压迫关节囊成葫芦形而妨碍股骨头复位。遇此应将髂腰肌在止点切断或作Z形延长[图1 ⑷],再切开关节囊狭窄部。然后,屈曲、外旋髋关节,从关节囊内显露并探查髋臼和其后上方的股骨头。股骨头多发育差而变形,软骨面色暗、无光泽、有不整齐的压迹,圆韧带被拉长并增粗。髋臼浅,臼内被脂肪、纤维组织和增生的软组织所充填,有时在臼缘上方有翻入臼内的盂唇软骨;在髋臼下缘有横韧带阻碍复位。所有影响股骨头复位的髋臼内充填物,均应予以切除,为股骨头复位准备条件[图1 ⑸ ⑹]。
 |
 |
| ⑸外旋下肢,显露关节腔 | ⑹清除髋臼内充填的组织 |
4.加深和扩大髋臼 髋臼面用刮匙或圆形髋臼锉去除一层软骨组织,加深和扩大髋臼,但以不露出骨面为度[图1 ⑺]。对不平整的股骨头软骨面,应予修圆;对股骨头较大不能适应髋臼者,可用球凹面髋臼锉磨去少许软骨面使之缩小。然后测量髋臼、股骨头的直径及深度,至二者相称时,才进行复位,使股骨头能稳定地存留在臼窝内。头大臼小时复位,必然头顶不能落入臼底,股骨头将不会稳定,日后有可能复发脱位,应予注意。
5.复位 内旋、伸直病肢,向下牵引,使股骨头还纳入髋臼内。试验股骨头在髋臼内的稳定性和软组织的紧张度,如中度屈髋和内收股骨头无脱位倾向,伸直位牵拉股骨头仅有少许松弛度,可认为复位比较稳定。即应由专人保持下肢于适度外展,内旋位,直至完成石膏固定,以防脱位。如需要其他辅助手术可于复位后进行。
 |
 |
| ⑺用髋臼锉加深髂臼 | ⑻复位关节,重叠缝合关节囊 |
| 图1 先天性髋关节脱位切开复位术 | |
6.缝合、外固定 上部关节囊的多余部分应予切除后缝合、或重叠缝合,以增强关节后上壁及关节的稳定性,消除复发的机会。然后,延长缝合髂腰肌腱,冲洗伤口,置胶管负压引流后按层缝合[图1 ⑻]。术毕即作病侧髋关节外展、内旋位的双侧髋人字石膏固定。石膏固定应松紧合适,以免术后关节再度脱位。
[术后处理]
1.严密观察病人血压、脉搏和呼吸情况。保证输液、输血通畅。注意观察下肢血运、神经功能。
2.术后3日摄片检查关节复位情况。如有脱位或复位、位置不佳,应研究、消除原因,调整位置或麻醉下手法复位,重新石膏外固定,甚至及早行二次切开复位等手术。
3.注意尿液处理,勿使浸湿石膏。石膏外固定于术后4~6周拆除,摄片复查情况良好者,应鼓励活动,髋、膝关节能屈曲90°后才下地逐渐负重。过早下地容易发生如股骨髁上骨折等并发症。最好在活动后第2周随诊一次,检查有无因肌力尚未恢复而活动过快的情况下发生股骨头外移现象。如发生这种情况,内旋髋即可纳入髋臼者,应用贝氏石膏短期固定锻炼,并严密观察。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







好详细,谢谢分享,好好学习!
80
好详细的手术介绍!学习了!梅斯医学真的是良心医学软件啊!
83
#关节脱位#
0
#先天性#
44
#脱位#
27