AHA 2017:基于证据的新治疗措施可改善NSTEMI患者预后——SWEDEHEART注册研究1995-2014结果公布
2017-11-19 天津医科大学总医院心内科 刘文楠 王清 杨清 壹生
本届AHA 2017科学年会上公布的SWEDEHEART注册研究结果表明:在过去20年中,NSTEMI患者远期预后的显着改善得益于院内介入治疗的广泛应用和基于循证医学的优化药物治疗。
新治疗方式对非ST段抬高型心肌梗死(NSTEMI)预后的改善究竟有多大影响?这个问题此前缺乏长期随访的大样本数据支持。本届AHA 2017科学年会上公布的SWEDEHEART注册研究结果表明:在过去20年中,NSTEMI患者远期预后的显着改善得益于院内介入治疗的广泛应用和基于循证医学的优化药物治疗。
SWEDEHEART注册研究纳入了1995年至2014年瑞典全国的几乎所有NSTEMI患者(n=205 693)。将所有患者以每2年一个区间进行分组,评价各组患者的基线资料、治疗情况和长期预后情况。使用COX回归模型以每2年为单位评价患者病情和治疗的变化对预后的影响。随着时间推移,伴随着基于循证医学证据的新治疗方法逐渐被采用,患者的预后显着改善。与对照人群相比,NSTEMI患者的标准化1年死亡率由1995/96年的5.53 (5.30~5.75)下降至2013/14年的3.03 (2.89~3.19)。经基线资料调整后,每2年的心脑血管死亡或心肌梗死事件呈线性下降(0.930,95%CI:0.926~0.935)。排除冠状动脉介入治疗的影响后,死亡率下降的趋势减弱(0.970,95%CI:0.964~0.975);进一步排除出院药物的影响后这种下降趋势几乎消失(0.988,95%CI:0.982~0.994)。
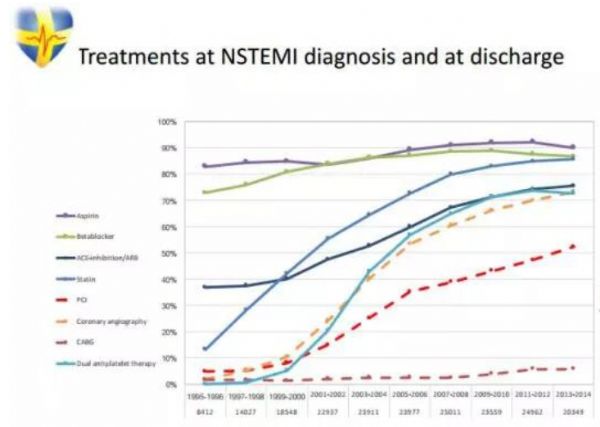
图1. 20年来NSTEMI治疗方式的变化
图2. 20年来NSTEMI预后的变化及治疗方式对预后的影响
尽管在长达20年的医学实践中,NSTEMI和心脏损伤的定义有所变化,而且冠状动脉介入和抗血小板治疗的进展无法分别评价,但作为整个国家层面长达20年的SWEDEHEART注册研究依然表明:过去20年,瑞典NSTEMI患者基于循证依据的新方法逐渐普及;患者的长期生存率显着提高,同时新发缺血性事件和心力衰竭的风险明显降低;这些进步被认为与院内介入治疗的广泛应用和基于循证医学的优化药物治疗有关;我们也期待继续推进基于最新指南推荐的优化治疗能进一步改善患者的预后。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#患者预后#
18
#NST#
28
#注册研究#
23
#结果公布#
17
#治疗措施#
39
#STEMI患者#
32
#AHA#
24
#ART#
25
#STEM#
25
#NSTEMI#
31