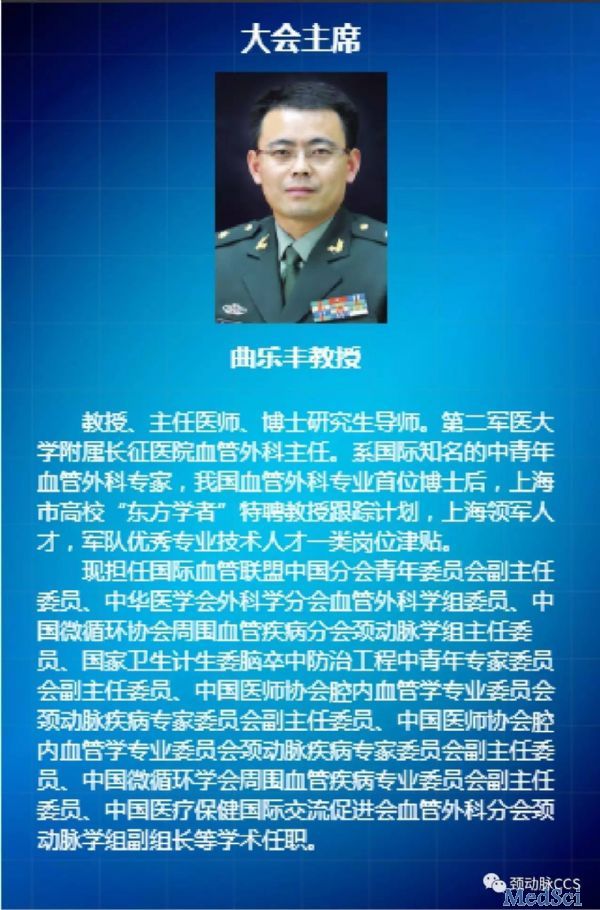
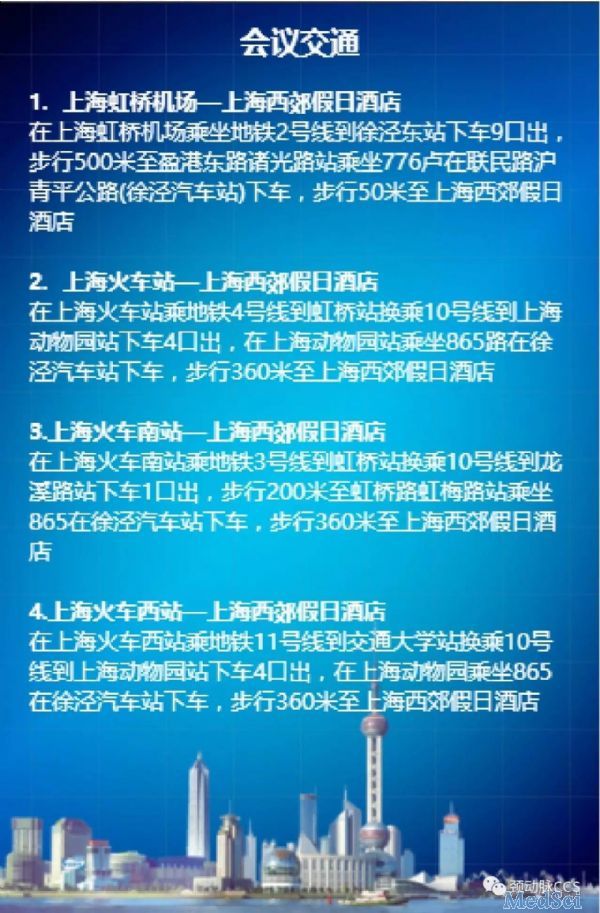
梅斯作为媒体参与第六届中华颈动脉外科高峰论坛 暨国际颈动脉外科峰会(CCS2017) 2017中国微循环学会周围血管疾病 专业委员会学术年会
2017-03-17 MedSci MedSci原创
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#学术年会#
39
#高峰论坛#
26
#ccs#
36
#微循环#
37
#颈动脉#
31
#梅斯#
29
#血管疾病#
31