Blood:外泌体在EBV相关性淋巴瘤的发展中发挥促炎性调控作用
2018-04-23 MedSci MedSci原创
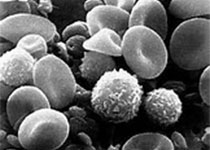
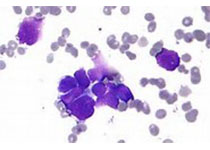
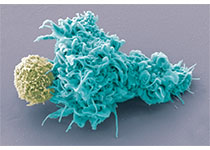
中心点:EBV编码miRNAs通过外分泌的方式从感染细胞转导至未感染细胞,从而调控肿瘤发生。EBV编码miRNAs可作为将EBV+ DLBCL患者分为两组的良好诊断标志物。摘要:老年人感染EB病毒(EBV)可引发多种疾病,包括B细胞淋巴瘤,如霍奇金淋巴瘤(HL)和弥漫性大B细胞淋巴瘤(DLBCL)。近日,Blood杂志上发表一篇文献,研究人员发现EB病毒可通过外分泌方式反式作用于肿瘤中的未感染的巨
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#促炎#
36
#相关性#
28
#EBV#
36
学习
70
学习学习谢谢
61
好
61