Heart:共病决定心动过缓起搏器置入患者预后
2013-08-29 高晓方 译 cmt
荷兰一项研究表明,置入前心衰病史、冠脉疾病和糖尿病为心动过缓起搏器置入者预后不佳的重要预测因素。论文8月22日在线发表于《心脏》(Heart)。此项前瞻性队列研究共纳入1517例接受首次心动过缓起搏器置入的患者。在常规临床条件下对患者进行随访,并评估患者起搏器置入前特征与生存率的相关性。主要转归指标为死亡原因和至死亡时间。结果显示,平均5.8年随访结束时共有512例(33%)患者死亡,大部分为非心
荷兰一项研究表明,置入前心衰病史、冠脉疾病和糖尿病为心动过缓起搏器置入者预后不佳的重要预测因素。论文8月22日在线发表于《心脏》(Heart)。【原文下载】
此项前瞻性队列研究共纳入1517例接受首次心动过缓起搏器置入的患者。在常规临床条件下对患者进行随访,并评估患者起搏器置入前特征与生存率的相关性。主要转归指标为死亡原因和至死亡时间。
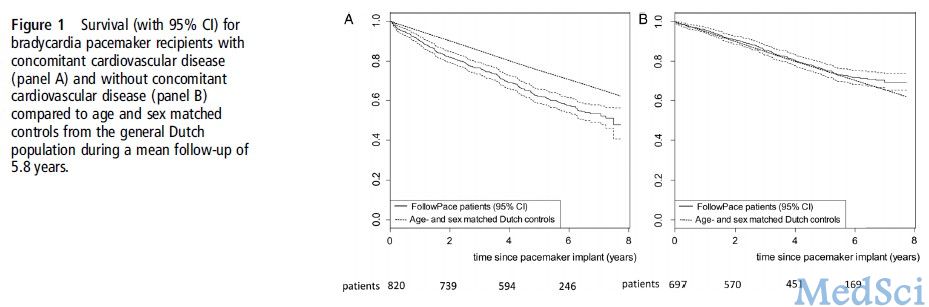
结果显示,平均5.8年随访结束时共有512例(33%)患者死亡,大部分为非心源性(67%)。起搏器相关性死亡为2例。1、3、5和7年时生存率分别为93%、81%、69%和61%。置入时无伴发心血管疾病的起搏器置入者在生存率方面与年龄、性别相匹配对照者相当。与心源性死亡相关的置入时预测因素包括年龄、冠脉疾病、糖尿病、心衰、瓣膜疾病和起搏器置入指证。全因死亡的预测因素包括男性、年龄、体质指数、冠脉疾病、心脏手术、糖尿病、心衰和维持性房室同步。
原始出处:
Udo EO, van Hemel NM, Zuithoff NP, Doevendans PA, Moons KG.Prognosis of the bradycardia pacemaker recipient assessed at first implantation: a nationwide cohort study.Heart. 2013 Aug 22. doi: 10.1136/heartjnl-2013-304445. 【原文下载】
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#患者预后#
35
#起搏器#
20
#ART#
24
#心动过缓#
33
#HEART#
26