NEJM:紫杉醇涂层装置增加周围动脉疾病的死亡率?
2020-12-10 MedSci原创 MedSci原创
周围动脉疾病是全球性的健康问题,其特征在于阻塞性动脉粥样硬化导致下肢血流量减少。 常常建议行血管内干预以防止截肢并减轻症状,但它们与手术后再狭窄的明显风险相关联,进而危及干
周围动脉疾病是全球性的健康问题,其特征在于阻塞性动脉粥样硬化导致下肢血流量减少。 常常建议行血管内干预以防止截肢并减轻症状,但它们与手术后再狭窄的明显风险相关联,进而危及干预的长期开放性。
紫杉醇(Paclitaxel)最初是从短叶红豆杉(Taxus brevifolia)树中分离出来的,它是一种疏水性的抗增殖剂,可用于已在欧盟批准的所有带药物涂层的气囊和支架,在美国可用于外周动脉疾病的干预措施。 药物涂层器械已被广泛应用于临床,可降低再狭窄的风险和重复干预的可能性,但它们对以患者为中心的临床终点如截肢率和生活质量的影响尚未得到证实。 瑞典在外周动脉疾病中的药物洗脱试验(SWEDEPAD)是一项基于注册中心的多中心,随机,开放标签的试验,旨在确定药物洗脱技术是否能够对患有慢性肢体缺血性心肌病和急性肢体缺血的患者的截肢率以及间歇性跛行患者的生活质量产生有利影响。
最近的一项荟萃分析表明,使用紫杉醇涂层装置可能导致晚期死亡风险增加。 这一发现引起了对涂层装置长期安全性的重大争议。SWEDEPAD试验的患者招募也因此于2018年12月10日暂停,该试验的数据和安全监控委员会建议,在相关患者的长期随访后,对所有原因的死亡率进行计划外的中期分析。

实验人员对临床试验的数据进行了计划外的中期分析。 在分析时,随机将2289例患者分配至两组——使用药物涂层器械治疗(药物涂层器械组1149例)或使用未涂层器械治疗(未涂层器械组1140例),随机分层则是根据疾病的严重程度即患者是否患有慢性肢体缺血(1480例)或间歇性跛行(809例)。 该中期分析的唯一终点是所有原因死亡率。
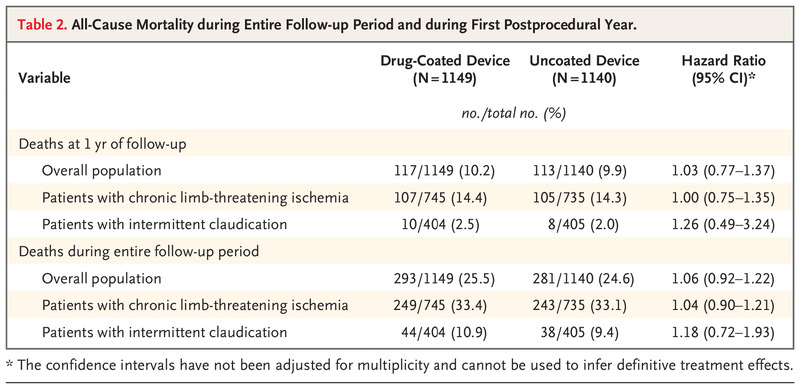
没有患者失去随访。 紫杉醇被用作所有药物涂层装置的涂层剂。 在平均2.49年的随访期间,有574例患者死亡,其中包括药物涂层器械组的293例(25.5%)和未涂层器械组的281例(24.6%)(危险比,1.06; 95% 置信区间为0.92至1.22)。 一年后,药物涂层器械组的全因死亡率为10.2%(117例患者),而未涂层器械组的全因死亡率为9.9%(113例患者)。 在整个随访期间,在慢性肢体缺血患者中,各治疗组之间的死亡发生率无显著差异(药物涂层装置组为33.4%[249名患者],无涂层器械组33.1%[243名患者])或间歇性跛行患者(分别为10.9%[44例]和9.4%[38例])。
在这项将紫杉醇涂层装置与未涂层装置用于外周动脉疾病血管内治疗的比较中的随机试验中,计划外的中期分析并未显示紫杉醇涂层装置的死亡率有明显升高。实验者认为,在试验完成之前发布这些总死亡率数据的有着重要意义:首先,他们试图减少患者和医生对紫杉醇涂层器械安全性的担忧;其次,对于那些仍在坚持紫杉醇涂层装置的积极作用的科研人员,这一结果有着至关重要的意义。
原文链接:https://www.nejm.org/doi/full/10.1056/NEJMoa2005206?query=featured_home
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#周围动脉疾病#
0
加油
85
赚积分
93
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
54
学习
93