Sci Adv:白血病药物联合PD-1抑制剂增强免疫治疗效果!
2019-02-25 疫苗 转化医学网
抗程序性死亡-1(PD-1)受体及其程序性死亡配体(PD-L1)的抗体药物,主要是通过克服患者体内的免疫抑制,重新激活患者自身的免疫细胞来杀伤肿瘤。
导 读
程序性细胞死亡蛋白-1(PD-1)及其配体(PD-L1)抗体是极具代表性的免疫检查点抑制剂,在癌症免疫治疗史中更是具有里程碑的意义。然而,PD-1抑制剂在未经选择的实体瘤患者中,有效率只有10%至30%,而起初具有良好治疗效果的患者,随着药物的长期使用也可能产生耐药。因此如何提高有效率及攻克其耐药性是国内外癌症专家共同关注和亟待解决的问题。
日前,西奈癌症中心的研究人员进行的一项新研究已经确定了一种药物--FDA批准的药物达沙替尼(dasatinib),极大地增强了抗PD-1治疗其他癌症的免疫疗法的治疗效果。他们的研究结果以“Targeting DDR2 enhances tumor response to anti–PD-1 immunotherapy”为题发表在《Science Advances》上。
抗程序性死亡-1(PD-1)受体及其程序性死亡配体(PD-L1)的抗体药物,主要是通过克服患者体内的免疫抑制,重新激活患者自身的免疫细胞来杀伤肿瘤。
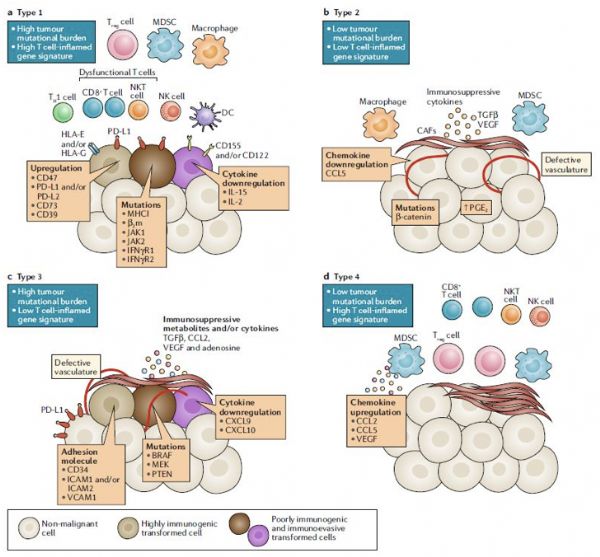
不可控的免疫反应或过度表达的自身抗原可引起炎性组织损伤和自身免疫性疾病,为了防止这种情况的发生,机体的免疫反应受到刺激和抑制信号之间的平衡调节,这些信号被统称为免疫检查点。
免疫检查点是免疫激活的重要调节因子,它们在维持免疫平衡和预防自身免疫性疾病中起着关键作用。活化的T细胞是免疫效应功能的主要介质。T细胞表达多个共抑制受体,如淋巴细胞活化基因3(lymphocyte-activation gene 3,LAG 3),PD-1和CTLA-4。机体利用这些免疫检查点分子来调节T细胞对自身蛋白、慢性感染以及肿瘤抗原的反应。不同免疫检查点分子的作用通路并不同。
早在去年,王洁教授团队利用TCGA和ICGC数据库,分析了不同DDR通路基因变异与TMB和新生抗原的关系,以及在免疫治疗疗效预测中的意义。DDR通路中任意一个基因突变被定义为该DDR通路突变,8条通路中任意一条通路突变与TMB和新抗原水平升高显着正相关。
单一DDR通路基因变异的中位TMB值为52(基于TCGA的WES数据),低于既往研究定义的TMB-H的水平。该研究将TMB前25%定义为TMB-H,通过ROC曲线发现,2条通路共突变时对TMB-H和新生抗原的预测灵敏度和约登指数最大,提示2条通路(DDR2基因)共突变可以更好的预测TMB-H和高的新抗原水平更高,免疫治疗获益可能性更高。
DDR2 是一种由纤维胶原蛋白激活的受体酪氨酸激酶, 因此在胶原细胞相互作用的调节中起着关键作用。DDR2通过诱导癌细胞扩散和生长来帮助肿瘤侵入健康组织。虽然其受到几种FDA批准的受体酪氨酸激酶抑制剂的抑制, 但由于达沙替尼在体外和体内都是DDR2最有效的抑制剂, 而且其在肿瘤临床试验中的使用情况也很普遍, 因此我们的研究中选择了达沙替尼。
研究人员发现,用达沙替尼来耗尽DDR2,他们能够通过结合两种药物来提高癌细胞对抗PD-1治疗的敏感性,这比单独使用两种药物要有效得多。候选基因DDR2通过shRNA介导的敲除和用dasatinib(达沙替尼)进行药理抑制试验。
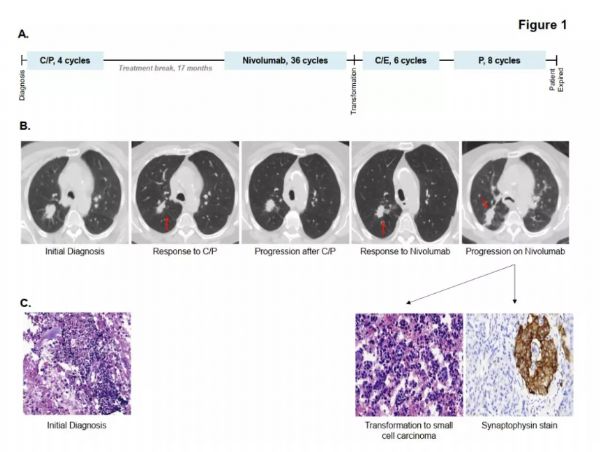
通过五种不同的肿瘤组织——膀胱、乳房、结肠、肉瘤和黑色素瘤——在小鼠体内的同种基因模型—研究表明,与单药治疗相比,DDR2的消耗增加了抗-PD-1治疗的敏感性。用抗-PD-1和DDR2酪氨酸激酶抑制因子dasatinib联合治疗肿瘤小鼠,导致了肿瘤负荷的降低。
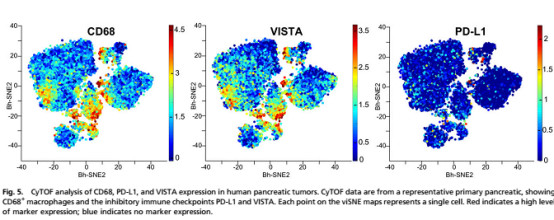
进一步探索发现,RNA-seq和CyTOF分析显示,在DDR2缺失的肿瘤中和联合抗-PD-1治疗的患者中,有较高的CD8+T细胞群。在这两种情况下,靶向DDR2和抗-PD-1治疗被证明是非常有效的跨多种不同类型的癌症在临床前的体内模型。
癌症的新一代免疫治疗方法突出了实验室发现的重要性,它们可以在临床上快速检测,跨越多种疾病类型,为患者提供免疫治疗本身可能无法达到的最佳效果。这项研究也为肿瘤免疫治疗提供了新的思路和方法,为提升治疗效果、改善疾病预后提供了非常有意义的参考和借鉴。
原始出处:Megan M. Tu, Francis Y. F. Lee, Robert T. Jones, et al. Targeting DDR2 enhances tumor response to anti–PD-1 immunotherapy. Science Advances 20 Feb 2019
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#白血病药#
32
#抑制剂#
25
#白血病药物#
43
#药物联合#
42
#治疗效果#
42
#PD-1抑制剂#
31
谢谢梅斯提供这么好的信息,学到很多
48
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
43