探案:这个隐藏很深的元凶,被TA轻易挖掘!
2018-12-17 骆煜、金文婷 SIFIC感染官微
2018年9月患者出现发热伴咳嗽,干咳为主,Tmax 38.4℃,无明显畏寒、寒战,无气促,至当地医院予抗感染治疗8天(具体不详),症状无明显好转。
一、病史简介
男性,51岁,安徽人,2018-11-15入中山医院感染病科
主诉:发热伴咳嗽2月
现病史:
2018年9月患者出现发热伴咳嗽,干咳为主,Tmax 38.4℃,无明显畏寒、寒战,无气促,至当地医院予抗感染治疗8天(具体不详),症状无明显好转。
2018-09-25至安庆某医院,查血WBC 3.50*10^9/L,N 26.7%,PLT 43*10^9/L,CRP 60.4mg/L,PCT 0.21ng/ml,胸部CT示两肺结节灶,转移待排;两肺炎症。予静滴哌拉西林他唑巴坦+莫西沙星+伏立康唑抗感染,辅以地塞米松治疗1周,发热、咳嗽症状逐渐好转,SpO2 98%左右,10-10出院。
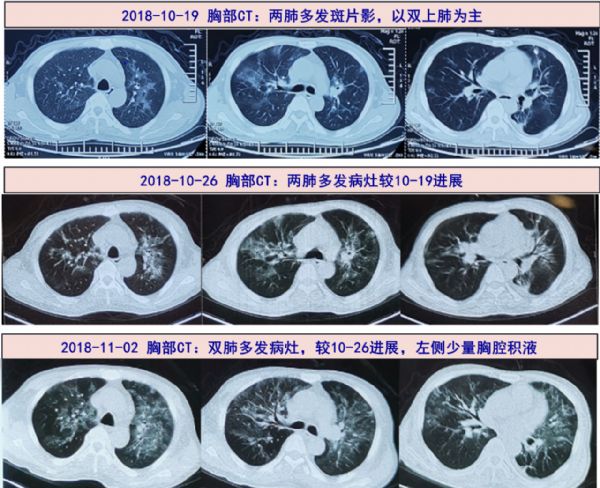
1周后再次发热、咳嗽,Tmax39.4℃,10-18再次至安庆医院就诊,查WBC 3.42*10^9/L,N 36.3%,PLT 77*10^9/L,CRP 59mg/L,胸部CT示两肺炎症。超声示双侧腋下肿大淋巴结。再次予静滴哌拉西林他唑巴坦+莫西沙星+伏立康唑抗感染,10-22复查血常规提示粒缺(WBC 1.3*10^9/L,N 0.5*10^9/L,PLT 62*10^9/L),仍发热咳嗽,并逐渐出现气促。
2018-10-23转至上海某三甲医院,查WBC 1.0*10^9/L,N 43.9%,PLT 39*10^9/L,CRP 27mg/L,PCT 0.05ng/ml,白蛋白25g/L,IgG 5g/L,BNP 702.5pg/ml,血培养、痰培养、GM、T-spot等检查均阴性;10-25胸部CT平扫:两侧肺门影大,两侧肺门旁多发斑片影,考虑感染性病变。予泰能+莫西沙星+伏立康唑抗感染,发热加重,Tmax40℃,伴气促,改用舒普深+两性霉素B治疗,并予益比奥+吉粒芬+特比奥升白升血小板、丙球、白蛋白、激素等治疗,气促加重。
2018-11-02复查胸部CT:较前片进展,加用更昔洛韦0.25g bid+SMZ 0.96g tid治疗,停用两性霉素B,改为氟康唑,同时予甲强龙40mg bid治疗。之后体温降至正常,咳嗽、气喘自觉较前略改善,分别于11-07/11-12随访WBC 2.97/3.7*10^9/L,PLT 33/45*10^9/L,CRP 29/7mg/L,PCT 0.05ng/ml,BNP 2366/1514 pg/ml。为明确诊断和进一步治疗,2018-11-15转入我院感染病科病房。
发病以来,患者精神、睡眠尚可,胃纳稍减退,大小便无殊,体重下降近10kg。
既往史及个人史:2017年3月外院诊断为外周T细胞淋巴瘤,曾行化疗6次(具体方案不详),2017年10月行自体干细胞移植,自述2018年3月复查超声提示有复发迹象,予口服西达本胺+来那度胺治疗,后患者反复出现发热、影像学示肺部感染(2018年5月曾予伏立康唑治疗,余诊疗不详)。2018年7月外院复查PET-CT及骨穿+活检提示淋巴瘤复发伴骨髓累及,于2018年8月底停药。30年前曾有肺结核病史,否认高血压、糖尿病、冠心病、肝炎病史等。
二、入院检查(2018-11-15)
体格检查
T 36.2℃, P 84bpm, R 20次/分, BP 140/92mmHg;口周疱疹已结痂,浅表淋巴结未及肿大。双肺呼吸音清,未及明显啰音。心律齐,未及杂音。腹平软,无压痛或反跳痛,双下肢无水肿。
实验室检查
血常规:Hb 91g/L,WBC 4.74X10^9/L,N 85%,L 13.1%,Plt 35X10^9/L
炎症标志物:hs-CRP 5.0mg/L,ESR 2mm/H,PCT 0.06ng/mL
尿常规及粪常规+OB:均阴性
肝肾功能:ALT/AST 24/11U/L,白蛋白 31g/L,Scr 47umol/L
心肌标志物:氨基末端利钠肽前体1037pg/ml
自身抗体、出凝血功能、甲状腺功能均正常
肿瘤标志物:CEA 18.4ng/mL,NSE 24ng/mL,余正常
血隐球菌荚膜抗原、肺炎支原体抗体、呼吸道病原体九联检:均阴性
G试验:1-3-β-D葡聚糖 44.8;T-SPOT A/B: 1/5
血培养、痰涂片+培养:阴性;
血气分析(不吸氧):PaO2 66mmHg,PaCO2 36mmHg,SpO2 94%;
细胞免疫检查:B淋巴细胞 CD19: 65.8%;T淋巴细胞 CD3: 32.4%;Th淋巴细胞 CD4: 27.8%;Ts淋巴细胞 CD8: 6.3%;CD4/CD8: 4.4;自然杀伤细胞(CD56+16): 1.2%
辅助检查
11-19 心电图:正常
11-19 腹部超声:脾肿大
11-21 超声心动图:升主动脉增宽
三、临床分析
病史特点:患者中年男性,发热伴咳嗽2月,干咳为主,后出现气促,外院胸部CT示:两肺多发斑片影,予以多种抗菌药物联合治疗,症状未见好转,肺部病灶逐渐进展。既往有外周T细胞淋巴瘤病史,曾行6次化疗、自体干细胞移植及靶向药物治疗。本次入院后查胸部CT示双肺多发片状渗出影(较前进展),CRP略有升高,血沉、PCT正常,血氧分压偏低,免疫球蛋白G及CD4+T淋巴细胞计数降低,G试验、血培养、痰涂片+培养、T-SPOT、自身抗体均阴性。疾病诊断和鉴别诊断考虑如下:
1、感染性疾病:考虑特殊病原体感染,主要为肺孢子菌和巨细胞病毒感染,普通细菌、非典型病原体(支原体和衣原体)和真菌(曲霉和念珠菌)感染的可能性小。
耶氏肺孢子菌肺炎(Pneumocystis jirovecii pneumonia,PJP ):常见于HIV、血液系统肿瘤、使用糖皮质激素和免疫缺陷的患者,主要表现为发热、干咳,伴呼吸困难,典型胸部影像学特征为双侧弥漫性的间质浸润。该患者表现及胸部CT与其相符,传统的确诊方法主要依赖于痰液或支气管肺泡灌洗液(BAL)显微镜下形态学检查,目前更多采用包括mNGS在内的核酸检测,敏感性较高。
病毒感染:本患者病程较长,无鼻塞流涕、头痛乏力、肌肉酸痛等症状,急性呼吸道病毒如流感病毒、鼻病毒和腺病毒感染可能性小。主要需考虑免疫抑制患者常见病毒如巨细胞病毒(CMV)和EB病毒引起的感染,确诊有赖于抗原抗体检测、病毒培养或核酸检测。
2、非感染性疾病:
淋巴瘤累及肺部:患者既往有外周T细胞淋巴瘤病史,2018年7月外院复查PET-CT及骨穿+活检提示淋巴瘤复发伴骨髓累及,曾予多种抗菌药物联合治疗,症状未见好转,肺部病灶有所进展,同时有粒细胞减少、血小板降低,故需考虑淋巴瘤进展、肺累及可能。
自身免疫疾病:常有多系统累及,呼吸系统主要表现为刺激性干咳、气急,伴低热,合并感染时可出现高热,合并有皮肤、关节等肺外病变,肺部可闻及Velcro啰音。该患者入院查自身抗体均阴性,CRP及血沉基本正常。
四、进一步检查、诊治过程和治疗反应
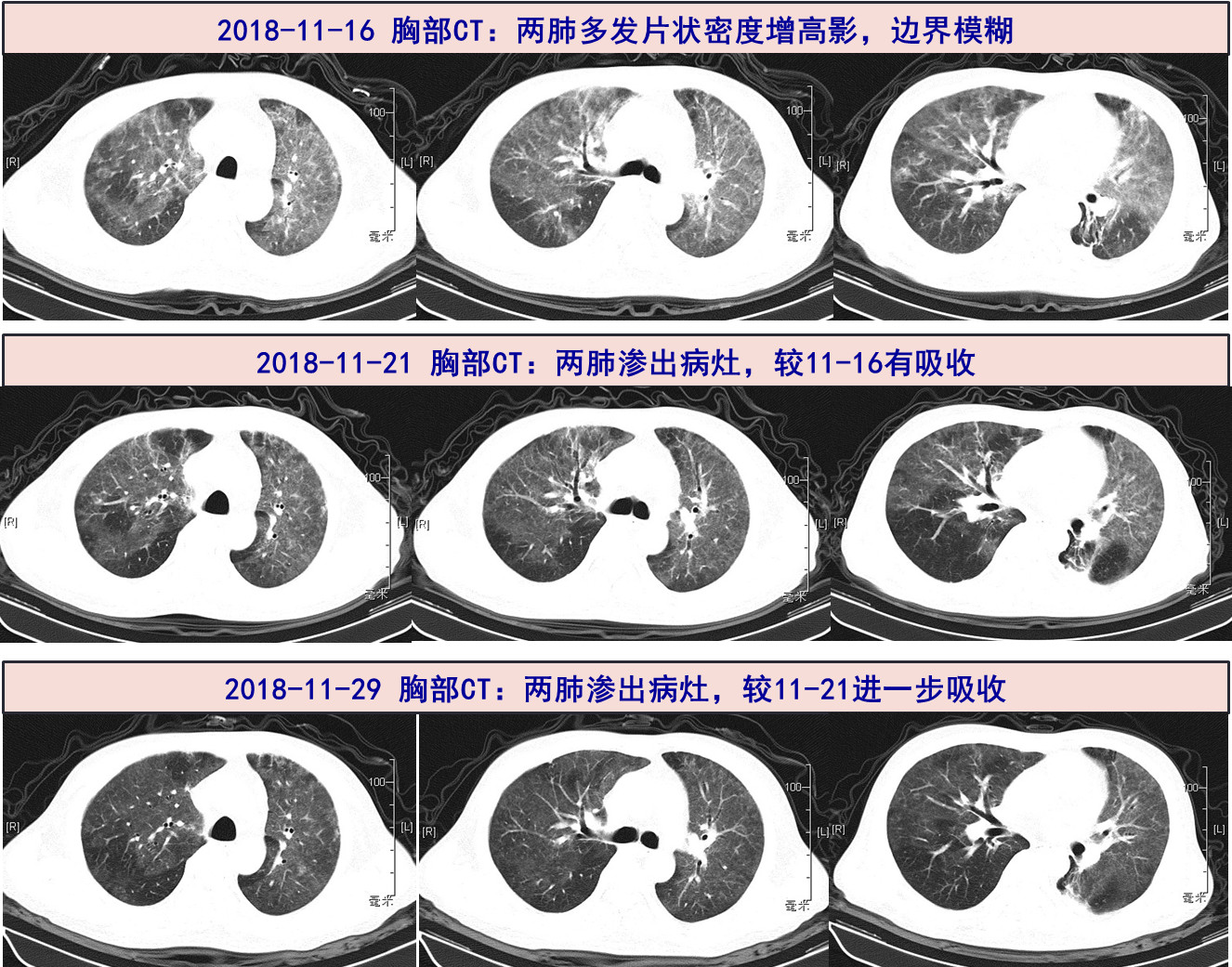
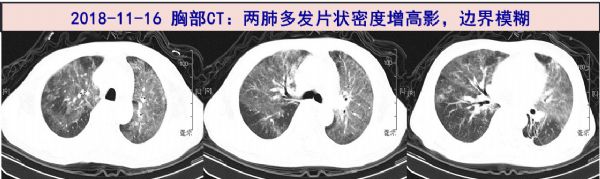
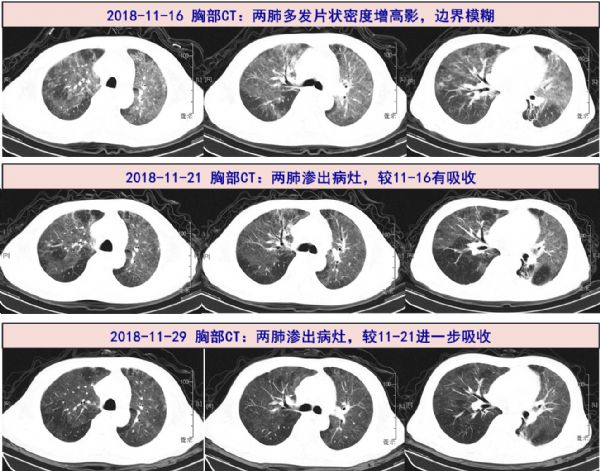
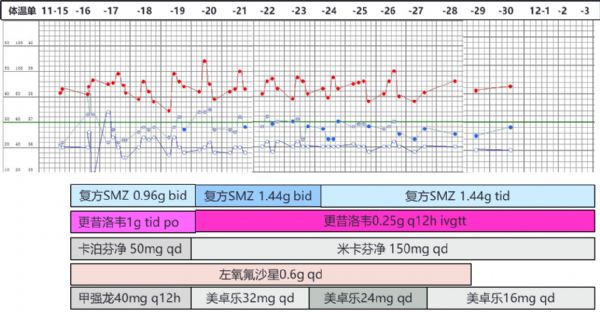
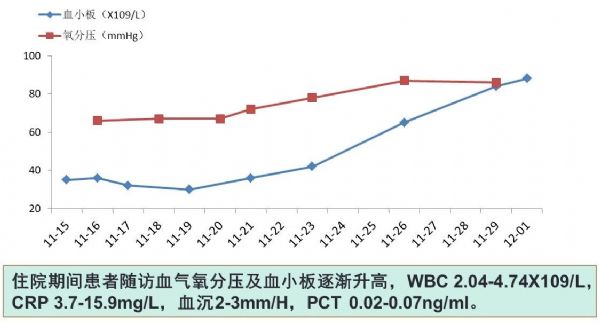
2018-11-16 复查胸部CT,示两肺毛玻璃样渗出病灶,较外院CT进一步加重,首先考虑PJP、合并病毒感染不除外,先前治疗效果不佳,考虑可能与SMZ剂量偏低有关,但因患者血小板偏低(35X10^9/L),予以复方SMZ 0.96g bid+卡泊芬净50mg qd联合抗PJP,更昔洛韦1g tid po抗病毒,加用左氧氟沙星0.6g qd以覆盖其他可能的病原体,同时予以甲强龙40mg q12h,升血小板等治疗, 密切监测血常规、血气分析。
2018-11-20 体温下降,气促较前缓解,痰液mNGS回报:检出序列为耶氏肺孢子菌、人类疱疹病毒5型(CMV)。调整抗感染方案为:复方SMZ 1.44g bid+静滴米卡芬净150mg qd+更昔洛韦0.25g q12h+左氧氟沙星0.6g qd,甲强龙减量至40mg qd、补充白蛋白、升血小板等治疗。
2018-11-21 血NGS回报亦提示耶氏肺孢子虫、CMV病毒。
2018-11-21 复查胸部CT提示两肺渗出病灶,较前前片(11-16)有所好转。
2018-11-23 复查WBC 2.16X10^9/L,血小板42X10^9/L,予调整复方SMZ为口服1.44g tid,口服甲泼尼龙片(美卓乐)32mg qd。
2018-11-29 复查胸部CT提示双肺病灶较前进一步好转,血小板升至84*10^9/L,随访动脉血气:PaO2 86.0mmHg,较前明显好转。停用左氧氟沙星,并逐渐调整美卓乐为16mg qd。继续口服复方SMZ 1.44g tid+静滴米卡芬净150mg qd+更昔洛韦0.25g q12h治疗。
2018-12-02 复查痰液mNGS回报:耶氏肺孢子菌及CMV核酸序列数,较11-16标本明显减少
体温及用药情况
五、最后诊断与诊断依据
最后诊断:
耶氏肺孢子菌肺炎(PJP)
巨细胞病毒肺炎
外周T细胞淋巴瘤
诊断依据:
患者中年男性,有淋巴瘤病史,化疗、自体干细胞移植术后,反复发热伴咳嗽2月,干咳为主,气促逐渐加重,胸部CT示:两肺多发斑片影,边界模糊,予以多种抗感染方案联合治疗,肺部病灶逐渐进展。入院后痰及血mNGS检测示:耶氏肺孢子菌、人类疱疹病毒5型(巨细胞病毒,CMV),予以复方SMZ+卡泊/米卡芬净+更昔洛韦、皮质激素等治疗后,体温降至正常、气促好转、血氧上升、胸部CT病灶逐渐吸收,复查痰mNGS检测肺孢子菌和CMV序列数明显降低,故考虑该诊断可以成立。
六、经验与体会
肺孢子菌肺炎(Pneumocystis pneumonia,PCP),又称为耶氏肺孢子菌肺炎(Pneumocystis jirovecii pneumonia,PJP),是由耶氏肺孢子菌(Pneumocystis jirovecii)引起,曾经被命名为卡氏肺孢子菌(Pneumocystis carinii),发生于免疫功能受损者,特别是HIV感染者、造血干细胞移植(HCT)和实体器官移植受者、血液系统恶性肿瘤,以及接受糖皮质激素、肿瘤化疗药物和其他免疫抑制药物的患者。病原学诊断和治疗耽误,可危及生命。该患者有外周T细胞淋巴瘤病史,曾行多次化疗、自体干细胞移植及靶向药物等治疗。本次入院查CD4+T淋巴细胞计数<200个/ul,属于PCP感染的高危人群。
PCP患者因免疫力低,通常合并多种病原体的感染,最常见合并的病毒为CMV、EBV。由于PCP临床表现缺乏特异性,传统确诊方法为痰液或BAL进行染色镜检,对检验人员的技术要求较高,非HIV感染的PCP患者体内肺孢子菌的负荷量较少,临床阳性诊断率更低。
值得指出的是,由于宏基因组的二代测序技术(mNGS)的推广应用,这个曾经被认为临床上获得病原学诊断十分困难的PCP,呼吸道标本(咳痰或BAL)甚至血液标本中,成功检出肺孢子菌已经变得轻而易举。另外,mNGS还可以同时识别多种病原体,对于混合感染的诊断具有重要意义,包括部分病毒如CMV和EBV。
PCP首选复方磺胺甲恶唑(TMP-SMX)治疗,肾功能正常患者的TMP-SMX剂量为15-20mg/(kg·d),分3次或4次静脉给药或口服。由于TMP-SMX的生物利用度极好,所以胃肠道功能正常的所有患者都适合口服给药。由于耶氏肺孢子菌囊壁含有β-D-葡聚糖,棘白菌素类能抑制其合成,故可作为PCP的治疗药物。文献显示部分重症病例可使用TMP-SMX联合棘白菌素类治疗。本例患者虽外院也曾予以复方SMZ+更昔洛韦治疗,但病情仍进展,入院后考虑复方SMZ剂量不足可能,但患者血小板低(35X10^9/L),复方SMZ可能出现进一步骨髓抑制,故联合棘白霉素类治疗,效果明显。
随着对非HIV感染者中PCP的临床认识不断提高,以及实验室诊断PCP方面的改善,非HIV感染者出现轻至中度PCP的情况近年来有增加趋势。该患者为自体HCT受者,属于PCP高风险人群,建议进行预防用药,推荐TMP-SMX作为一线用药。研究发现,与不预防或使用氟喹诺酮类药物(对肺孢子菌无效)预防相比,TMP-SMX预防使PCP发生减少了85%(RR 0.15,95%CI 0.04-0.62),PCP所致死亡率也显着降低(RR 0.17,95%CI 0.03-0.94)。非HIV感染者通常能良好耐受TMP-SMX,仅3.1%的成人出现了需停止治疗的不良事件,如白细胞减少、血小板减少、重度皮肤反应等。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









mark
49
学习谢谢分享
59
不错不错
64
很好的学习机会
57
长见识了,学习学习
66
好好好好好好好好
19