RNAi疗法givosiran治疗急性肝性卟啉症的晚期研究达到主要终点
2019-03-07 不详 网络
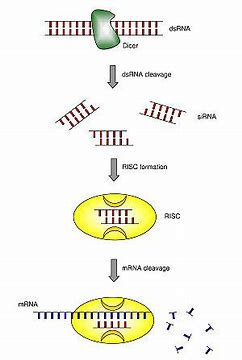
Alnylam制药本周三(2019年3月6日)报道,用于治疗急性肝性卟啉症(AHP)的研究性RNAi疗法givosiran的III期研究符合其主要疗效终点和许多次要目标。
Alnylam制药本周三(2019年3月6日)报道,用于治疗急性肝性卟啉症(AHP)的研究性RNAi疗法givosiran的III期研究符合其主要疗效终点和许多次要目标。该公司表示,根据ENVISION试验的最佳结果,它计划在2019年中期向FDA提交营销申请并在欧洲提交申请。该试验随机分配了94例AHP患者,其中89例患有基因证实的急性间歇性卟啉症(AIP),这些患者接受了针对氨基乙酰丙酸合成酶1的givosiran或安慰剂治疗。该研究的主要终点为复合性卟啉症发作的年化率的降低。该研究的结果显示,与安慰剂相比,givosiran达到了降低复合性卟啉症发病年率的主要目标,并且在9个次要终点中的5个中取得了显著结果。
卟啉症是因为人体内的卟啉(Porphyrin)等物质异常累积所造成的身体病变。人体以卟啉为前驱物,透过特定酶的催化作用来制造血红素,一旦酶无法正常作用,卟啉等物质便会越积越多,最终引致卟啉症。卟啉症是一种罕见疾病,临床统计估计发生机率约30万分之1,目前仍无治愈方法,只能针对卟啉症的病征进行治疗。
原始出处:
http://www.firstwordpharma.com/node/1628182#axzz5hUFjzudx
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#主要终点#
36
#givosiran#
38
#RNAi#
30