病例1
【一般资料】
男,46岁
【主诉】
因雷电击伤后意识不清4h入院。
【现病史】
当地医院头部CT示双侧基底节区出血,对症处理后转入我院。
【体格检查】
神志浅昏迷;部分头发烧焦;双侧瞳孔等大等圆,直径2mm,对光反射迟钝,眼球浮动;疼痛刺激后,四肢略屈曲回缩;双上肢可见6%Ⅲ度烧伤创面,表面污秽,大部分创面红白相间,右手掌心见长约5.0cm创口,深及掌腱膜,无明显活动性出血;肢体肿胀不明显,末梢循环良好。
【辅助检查】
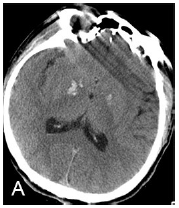
入院后复查头部CT示双侧基底节区高密度影,无明显占位效应,脑室系统无明显变化(图1A)。急诊生化检查示:丙氨酸氨基转移酶53U/L(正常范围:9~50U/L),门冬氨酸氨基转移酶81U/L(正常范围:15~40U/L),γ-谷氨酰胺转肽酶77U/L(正常范围:10~60U/L),肌酸激酶620U/L(正常范围:38~174U/L),肌酸激酶同工酶52U/L(正常范围:0~45U/L),乳酸脱氢酶868U/L(正常范围:313~618U/L)。
【初步诊断】
雷电击伤,双侧基底节区出血,6%双上肢Ⅲ°电击伤。
【治疗】
入院后予以低流量吸氧,心电监护,生理盐水补充血容量;同时,应用碳酸氢钠碱化尿液,甘露醇降颅内压及利尿;行创面清创术,预防注射破伤风抗毒素3000U;应用氨甲环酸止血、醒脑静促醒、奥美拉唑抑酸、复方磺胺嘧啶锌凝胶创面外用预防感染。病情稳定后,行康复治疗。治疗1周后复查头部CT示出血少量吸收,无脑积水(图1B)。出院时,意识清楚,创面愈合良好,四肢侧肢体肌力4级,肌张力正常,生活可自理。

病例2
【一般资料】
男,50岁,
【主诉】
因雷电击伤后意识不清伴左侧肢体活动障碍4d入院。
【现病史】
当地医院头部CT示右侧基底节区出血破入脑室。对症处理后转入我院。
【体格检查】
神志嗜睡;头皮无裂伤、挫伤和血肿,头发完整;双侧瞳孔等大等圆,直径3mm,对光反射灵敏;右侧肢体肌力4级,左侧肢体肌力2级,肌张力未见异常,左侧腱反射亢进;右侧颈部、躯干、右上肢、会阴见9%深Ⅱ度烧伤创面,渗出明显;右上肢浮肿,末梢循环尚可。
【辅助检查】
入院后头部CT示右侧基底节区不规则高密度影,稍有占位效应,同侧脑室系统稍有受压(图2A)。急诊生化检查示:丙氨酸氨基转移酶48U/L,门冬氨酸氨基转移酶42U/L,γ-谷氨酰胺转肽酶121U/L,肌酸激酶355U/L,肌酸激酶同工酶9U/L,乳酸脱氢酶965U/L。

【初步诊断】
雷电击伤,右侧基底节区出血破入脑室,右侧颈部、躯干、右上肢、会阴9%深Ⅱ°电击伤。
【治疗】
入院后予以低流量吸氧,心电监护,生理盐水补充血容量;同时,应用碳酸氢钠碱化尿液,甘露醇降颅内压及利尿;创面清创,预防注射破伤风抗毒素3000U,复方磺胺嘧啶锌凝胶创面外用预防感染;应用氨甲环酸止血、奥美拉唑抑酸防治应激性溃疡;应用神经营养、促醒、抗氧化剂维生素C等药物。病情稳定后,行康复治疗。治疗3周后复查头部CT示出血基本吸收,无脑积水(图2B)。出院时,意识清楚,创面愈合良好,左侧肢体肌力5级,生活自理。

【讨论】
雷电击伤致颅内出血的病理生理学机制仍不清楚,主要由以下几种可能:①高压电流直接热灼损伤,致脑血管破裂出血;②基底节本身血供较差,侧支循环较少,变异较多,在血管病变的基础上血压升高及供血动脉的扭曲、牵拉、移位,导致血管破裂出血;③雷电击伤后意识不清,跌倒摔伤,从而形成基底节区出血;④强烈的周围血管收缩致精神紧张、情绪激动等导致血压的骤然升高,诱发血管破裂出血。肢体与肢体的放电在大脑中不产生电流,所以直接脑损伤的发生必须要闪电击中头部。电流会通过阻力最小的径路从直立受害者的身体和腿传导到地上。血管和神经组织与其他组织相比,在单位面积上可运载更多的电流,在周围组织受损之前已受损。血管周围间隙(Virchow-Robinspaces,VRS)是蛛网膜的软脑膜随着穿通动脉和流出静脉进出脑实质的延续,直至毛细血管水平。在脑内、软脑膜下腔和蛛网膜下腔的小动脉和微小动脉周围包绕着由软脑膜细胞形成的血管周围鞘,脑内动脉的血管周围间隙与蛛网膜动脉的血管周围间隙直接相连,随着豆纹动脉通过前穿质进入基底节区,因此,VRS在雷击后的基底节损伤中起着重要作用。本文2例雷电击伤主要表现为基底节区出血。严重的雷电击伤应迅速建立生命通道,立即展开快速液体复苏,争取在较短的时间内满足组织的灌注,特别是脑、心、肾脏等的有效灌注。渗透性利尿和碱化尿液为预防急性肾功能衰竭所必需。同时,甘露醇的早期应用,不仅有解除肾血管痉挛,消除肾小管细胞和肾间质水肿,防止管型形成的作用,而且还能防治脑水肿和改善肺功能。由于甘露醇能减轻组织水肿和上皮细胞的肿胀,减轻血管阻力而增加血流,因此能改善循环及代谢,有利于组织的修复。雷击伤致颅内出血,病情变化快,病死率高,因此,在雷击伤的治疗过程中应注意进行头颅CT检查并采取预防措施,一旦出现突发昏迷,均应进行头颅CT检查和积极抢救。
原始出处:
李敬文, 胡永珍, 王开乐,等. 雷电击伤致基底节区出血2例[J]. 中国临床神经外科杂志, 2017(2):119-120.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







好文献.学习了
62
好文献学习了
66
#基底节#
40
病例比较罕见.值得学习学习
54
谢谢分享.学习了
55