NEJM:丛林地散步,需谨慎莱姆病!
2015-05-29 MedSci MedSci原创
一个8岁的男孩因眼眶周围皮疹10余天到院就诊,而在这之前曾有过膝关节疼痛,发烧,头痛的症状。据男孩的家长称,男孩在3周前在森林散步时右膝盖后边的腘窝部位曾被2只蜱咬伤,蜱虫是在2天后发现才取出的。 经体格检查,可见眼眶周围有游走性的红斑现象(如图A和图B所示),其他部位如右膝前、右边腋下和臀部亦可见此迹象。血清学检验发现伯氏疏螺旋体IgG抗体水平为0.58(正常值<0.20),伯氏疏螺
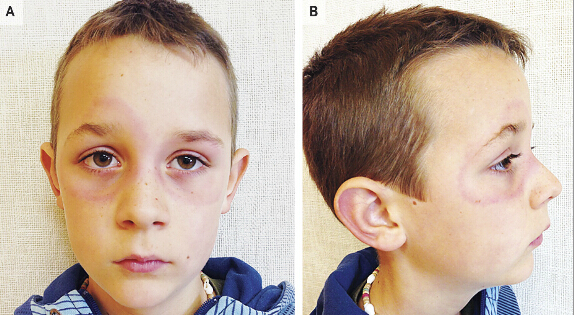
一个8岁的男孩因眼眶周围皮疹10余天到院就诊,而在这之前曾有过膝关节疼痛,发烧,头痛的症状。据男孩的家长称,男孩在3周前在森林散步时右膝盖后边的腘窝部位曾被2只蜱咬伤,蜱虫是在2天后发现才取出的。
经体格检查,可见眼眶周围有游走性的红斑现象(如图A和图B所示),其他部位如右膝前、右边腋下和臀部亦可见此迹象。血清学检验发现伯氏疏螺旋体IgG抗体水平为0.58(正常值<0.20),伯氏疏螺旋体IgG抗VIsE水平为每升75.5kU(正常水平,<16),和莱姆病螺旋体IgM抗体水平为5.85(正常值,<0.20)。免疫印迹检测结果显示B. garinii IgG和IgM抗体为阳性。这些检查结果证实了该男孩确诊为莱姆病。
最后,主治医生对这名男孩采用阿莫西林进行治疗3周,现症状已消失并康复出院。
关于莱姆病---
莱姆病是一种以蜱为媒介的螺旋体感染性疾病。我国于1985年首次在黑龙江省林区发现本病病例,以神经系统损害为该病最主要的临床表现。其神经系统损害以脑膜炎、脑炎、颅神经炎、运动和感觉神经炎最为常见。其中一期莱姆病仅用抗生素即可奏效,至二期、三期用抗生素无济于事,特别是神经系统损害更乏特效疗法。早期以皮肤慢性游走性红斑为特点,以后出现神经、心脏或关节病变,通常在夏季和早秋发病,可发生于任何年龄,男性略多于女性。发病以青壮年居多,与职业相关密切。以野外工作者、林业工人感染率较高。据报道疫区室外工作人员劳动一天后有40%被蜱叮咬史,或可从其皮肤、衣服等处找到蜱。室外消遣活动如狩猎、垂钓和旅游等均可增加感染莱姆病的危险性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









。
118
看看
75
#莱姆病#
27
多关注
167
预防为先
102
预防为主
93
国内也多
130