JACC:分流术类型对于Fortan治疗前有单右心室异常患儿的心脏大小和功能的影响
2014-12-01 MedSci译 MedSci原创
背景:在患有单右心室(RV)异常改变的儿童中,右心室的大小和功能可能受Norwood程序中选择的分流类型的影响。 目的:研究试图确定在Norwood治疗幸存者中接受14个月和小于等于6个月的前房坦治疗患者的超声心动图的区别。 方法:我们对比了两组病人2维多普勒超声心动的右心房大小和功能的指数,新主动脉环和三尖瓣环的尺寸和功能,主动脉尺寸,以及 14.1±1.2个月和33.6±9.6个月
背景:在患有单右心室(RV)异常改变的儿童中,右心室的大小和功能可能受Norwood程序中选择的分流类型的影响。
目的:研究试图确定在Norwood治疗幸存者中接受14个月和小于等于6个月的前房坦治疗患者的超声心动图的区别。
方法:我们对比了两组病人2维多普勒超声心动的右心房大小和功能的指数,新主动脉环和三尖瓣环的尺寸和功能,主动脉尺寸,以及 14.1±1.2个月和33.6±9.6个月的血管通畅程度。这两组接受诺伍德程序治疗的患者,分别被随机分配到Blalock-Taussig分流术(MBTS)和右心室-肺动脉分流术(RVPAS)。
结果:在两个时间段有240名患者可以做超声心动图(114 MBTS ,126 RVPAS)。 在14个月时,两组所有的指数都相似。从 14个月到前房坦治疗的超声心动图,MBTS组有稳定的右心室体积分数指数RV和心脏射血分数,而rvpas组右心室体积增加(P = 0.004),右心室射血分数减少(P = 0.004)。从14个月到前房坦治疗,两组的主动脉瓣区指数,轻度主动脉瓣回流(<5 % 每次)指数,三尖瓣指数和轻度三尖瓣回流(<20% 每次),均相似。
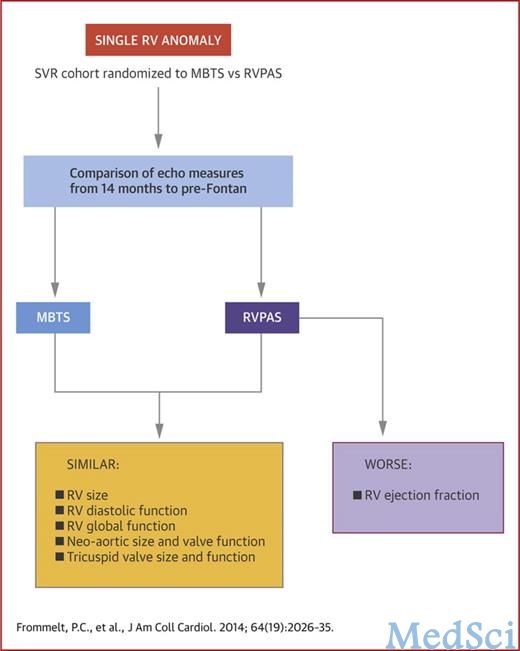
结论:在单右心室异常患病者换把第二年和第三年,右心室射血分数恶化后,初始诺伍德治疗的分流术类型影响预房坦的右心室重塑。可喜的是,不论哪种分流类型,右心室其他指标保持稳定,在房坦之前。(对比两种分流对单心室缺陷患儿进行分阶段重建的影响--小儿心脏网;nct00115934)
原始出处:
Peter C. Frommelt, MD; Eric Gerstenberger, MS; James F. Cnota, MD; Meryl S. Cohen, MD; Jessica Gorentz, RDCS; Kevin D. Hill, MD, MS; J. Blaine John, MD; Jami C. Levine, MD; Jimmy Lu, MD; William T. Mahle, MD; Rachel T. McCandless, MD; Luc Mertens, MD, PhD; Gail D. Pearson, MD, ScD; Carolyn Spencer, MD; Deepika Thacker, MD; Ismee A. Williams, MD, MS; Pierre C. Wong, MD; Jane W. Newburger, MD, MPH.Impact of Initial Shunt Type on Cardiac Size and Function in Children With Single Right Ventricle Anomalies Before the Fontan ProcedureThe Single Ventricle Reconstruction Extension Trial.J Am Coll Cardiol. 2014;64(19):2026-2035. doi:10.1016/j.jacc.2014.08.033
本文是MedSci原创编译整理,欢迎转载!转载请注明来源并附原文链接。谢谢!
您还可以这样阅读,更多资讯,请关注MedSci微信


版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#JACC#
34
#ACC#
30
#右心室#
36