JACC:先兆子痫病史是年轻女性冠状动脉粥样硬化的独立危险因素
2022-06-13 MedSci原创 MedSci原创
先兆子痫病史是年轻女性冠状动脉粥样硬化的一个独立的危险因素
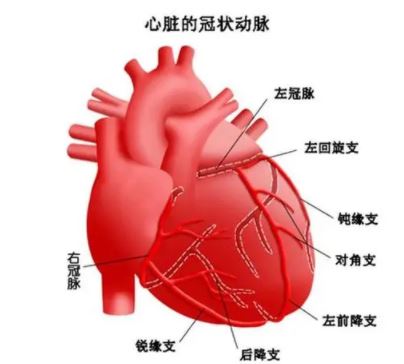
在过去的几十年中,与冠状动脉疾病 (CAD) 相关的死亡率有所下降。但是,这种可喜的趋势并没有在年轻女性身上观察到。实际上,据报道显示,55岁以下年轻女性的急性冠状动脉综合征发生率不降反增,特别是有过先兆子痫病史的妇女。
本研究旨在明确有先兆子痫病史的年轻女性冠状动脉粥样硬化的患病率,并与普通人群的女性进行比较。
纳入了40-55岁既往有先兆子痫病史的女性,同时1:1匹配纳入普通人群女性。受试者完成了广泛的问卷调查、临床检查和冠状动脉计算机断层血管造影(CTA)。主要终点是冠状动脉CTA查出的任何冠状动脉粥样硬化的患病率,或在非诊断冠脉CTA的情况下,钙评分>0。
两组女性冠状动脉粥样硬化的发生率
共纳入了1417位女性,平均47岁,其中708位既往有先兆子痫病史,709位来自普通人群。既往有先兆子痫病史的女性更可能有高血压(20.1% vs 22.8%,p<0.001)、血脂异常(47.7% vs 41.7%,p=0.023)、糖尿病(3.4% vs 1.1,p=0.004)和高体重指数(27.3±5.7 vs 25.0±4.2kg/m2,p<0.001)。
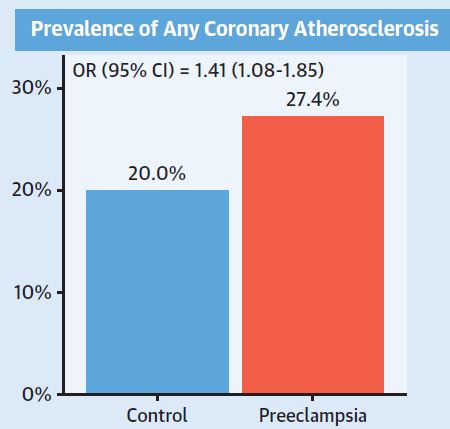
所有受试者都进行了心脏计算机断层扫描。根据年龄、血脂异常、糖尿病、体重指数、绝经校正后,既往有先兆子痫病史的女性存在任何冠状动脉粥样硬化的概率显著高于对照组(27.4% vs 20.0%,p=0.001;优势比[OR] 1.41,p=0.012)。
综上所述,与普通人群女性相比,既往有过先兆子痫病史的年轻女性发生冠状动脉粥样硬化的概率更高。根据传统的心血管危险因素调整后,子痫前期仍是冠状动脉粥样硬化的一个独立的危险因素。
原始出处:
Hauge Maria G,Damm Peter,Kofoed Klaus F et al. Early Coronary Atherosclerosis in Women With Previous Preeclampsia.[J] .J Am Coll Cardiol, 2022, 79: 2310-2321. https://doi.org/10.1016/j.jacc.2022.03.381
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#粥样硬化#
66
#独立危险因素#
40
#JACC#
65
#ACC#
39
#年轻女性#
81