Nature:研究人员利用小分子RNA诱导心脏组织再生
2013-05-06 Beyond 生物谷
引入两个小分子RNA导致心脏组织再生,近日,意大利国际遗传工程和生物技术中心研究小组已成功诱导了小鼠受损心脏组织再生。相关研究结果刊登在Nature杂志上。 由于心脏组织不能自然再生,出生后不久细胞就会停止增殖,研究人员一直在寻找一种手段能人为地诱导心脏组织再生。 迄今为止,还没有找到方法修复受到损害的心脏。为了要找出哪些microRNAs是导致心脏细胞分裂的因素,他们利用人心脏组织来源的mi
引入两个小分子RNA导致心脏组织再生,近日,意大利国际遗传工程和生物技术中心研究小组已成功诱导了小鼠受损心脏组织再生。相关研究结果刊登在Nature杂志上。
由于心脏组织不能自然再生,出生后不久细胞就会停止增殖,研究人员一直在寻找一种手段能人为地诱导心脏组织再生。
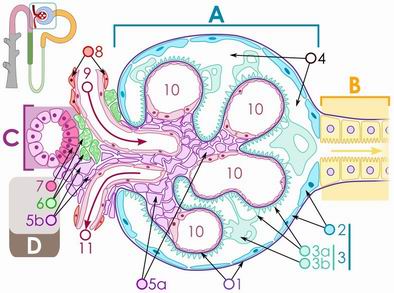
迄今为止,还没有找到方法修复受到损害的心脏。为了要找出哪些microRNAs是导致心脏细胞分裂的因素,他们利用人心脏组织来源的microRNAs植入到啮齿动物肌肉中,研究小组对875个microRNAs进行了分析研究。他们发现他们其中204能强烈激活细胞增殖。然后,他们选择了两个作用最强的,并用一种无害病毒作为载体将其注射到活体小鼠中,结果能引起他们受损害心脏组织再生。
两个星期后,被注射了小分子RNA的小鼠心脏表现出了比治疗前较少的伤害,这表明心脏组织再生确实发生了。两个月后,受损组织的面积已经减少了一半。该小组还指出,心脏收缩强度以及其他心脏功能均有所提高。
该研究小组得出结论,在不久的将来,利用小分子RNA诱导受损心脏组织再生可能被用来治疗心脏疾病受害者,但他们也指出必须进行更多的研究,因为此方法可导致细胞分裂有时会引发肿瘤。

doi:10.1038/nature11739
PMC:
PMID:
Functional screening identifies miRNAs inducing cardiac regeneration
Ana Eulalio,Miguel Mano,Matteo Dal Ferro,et al.
In mammals, enlargement of the heart during embryonic development is primarily dependent on the increase in cardiomyocyte numbers. Shortly after birth, however, cardiomyocytes stop proliferating and further growth of the myocardium occurs through hypertrophic enlargement of the existing myocytes. As a consequence of the minimal renewal of cardiomyocytes during adult life, repair of cardiac damage through myocardial regeneration is very limited. Here we show that the exogenous administration of selected microRNAs (miRNAs) markedly stimulates cardiomyocyte proliferation and promotes cardiac repair. We performed a high-content microscopy, high-throughput functional screening for human miRNAs that promoted neonatal cardiomyocyte proliferation using a whole-genome miRNA library. Forty miRNAs strongly increased both DNA synthesis and cytokinesis in neonatal mouse and rat cardiomyocytes. Two of these miRNAs (hsa-miR-590 and hsa-miR-199a) were further selected for testing and were shown to promote cell cycle re-entry of adult cardiomyocytes ex vivo and to promote cardiomyocyte proliferation in both neonatal and adult animals. After myocardial infarction in mice, these miRNAs stimulated marked cardiac regeneration and almost complete recovery of cardiac functional parameters. The miRNAs identified hold great promise for the treatment of cardiac pathologies consequent to cardiomyocyte loss.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Nat#
34
#研究人员#
36
#小分子#
38
#组织再生#
40