AHA 2016:他汀类药物能改善心脏骤停患者的生存结局
2016-11-15 MedSci MedSci原创
根据在美国心脏协会科学会议上发表回顾性队列研究结果,对于院外心脏骤停患者,心脏骤停前使用他汀类药物与不使用他汀类药物比较,患者有更好的生存结局。 研究人员报告说,在糖尿病患者中,这种影响是特别明显的。 来自台湾的研究人员Ping-Hsun Yu博士和同事推测,心脏骤停前使用他汀类药物可能会改善结局,因为他汀类药物具有多效性,包括减少炎症相关的损伤和内皮功能障碍。 研究纳入了137
根据在美国心脏协会科学会议上发表回顾性队列研究结果,对于院外心脏骤停患者,心脏骤停前使用他汀类药物与不使用他汀类药物比较,患者有更好的生存结局。
研究人员报告说,在糖尿病患者中,这种影响是特别明显的。
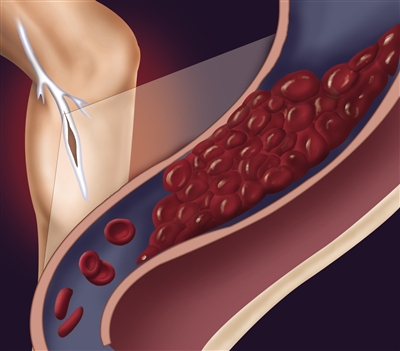
来自台湾的研究人员Ping-Hsun Yu博士和同事推测,心脏骤停前使用他汀类药物可能会改善结局,因为他汀类药物具有多效性,包括减少炎症相关的损伤和内皮功能障碍。
研究纳入了137933名年龄18岁及以上的患者,他们的心脏骤停与创伤无关。其中9059名患者在心脏骤停前至少90天内使用了他汀类药物。使用倾向匹配方法,比较了8249名心脏骤停前服用了他汀类药物与24747没有服用他汀类药物患者的生存结局。
与没有服用他汀类药物的患者比较,心脏骤停前服用了他汀类药物的患者入院时有更高的生存率(OR = 1.19; 95% CI, 1.12-1.27),活着出院的可能性更大(OR = 1.47; 95% CI, 1.31-1.65),1年生存率更高(OR = 1.5; 95% CI, 1.31-1.71)。
当研究人员构建了一个logistic回归模型后,他们发现,心脏骤停前服用了他汀类药物是心脏骤停后1年生存率的独立预测因子(OR = 1.45; 95% CI, 1.26-1.68)。
根据亚组分析结果,他汀类药物对糖尿病患者心脏停搏后存活率的影响尤其显著。
原始出处:
Yu PH, et al. Presentation 15. Presented at: American Heart Association Scientific Sessions; Nov. 12-16, 2016; New Orleans.
Statin use confers better outcomes after cardiac arrest, particularly in patients with diabetes.Healio.November 14, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#他汀类药#
20
这是一项回顾性的研究还是前瞻性研究?
58
#AHA#
28
不知道,文献中可以找到具体时间,先Mark一下,后面细读
50
学习了啊
64
怎么及时在骤停前给药呢?
58