更新版预混胰岛素临床应用专家共识出炉,抓紧拿走!
2016-09-11 佚名 药品评价
中国新诊断的2型糖尿病(T2DM)患者以餐后血糖升高为主,这可能与中国患者胰岛β细胞功能的衰退更显著、饮食结构多以碳水化合物为主有关。预混胰岛素能同时提供基础和餐时胰岛素,控制餐后血糖同时兼顾整体血糖。因此,目前多数中国T2DM患者选择预混胰岛素为胰岛素起始治疗方案。为了更好地指导临床医生合理规范使用预混胰岛素,中华医学会内分泌学分会于2013年发表了《预混胰岛素临床应用共识》,考虑到三年来有
中国新诊断的2型糖尿病(T2DM)患者以餐后血糖升高为主,这可能与中国患者胰岛β细胞功能的衰退更显著、饮食结构多以碳水化合物为主有关。预混胰岛素能同时提供基础和餐时胰岛素,控制餐后血糖同时兼顾整体血糖。因此,目前多数中国T2DM患者选择预混胰岛素为胰岛素起始治疗方案。
为了更好地指导临床医生合理规范使用预混胰岛素,中华医学会内分泌学分会于2013年发表了《预混胰岛素临床应用共识》,考虑到三年来有一些临床研究证据的更新,故基于原共识进行重新修订,形成预混胰岛素临床应用专家共识(2016年版)以下是主要内容:
1、预混胰岛素分类
预混胰岛素主要包括预混人胰岛素和预混胰岛素类似物(见表1)。
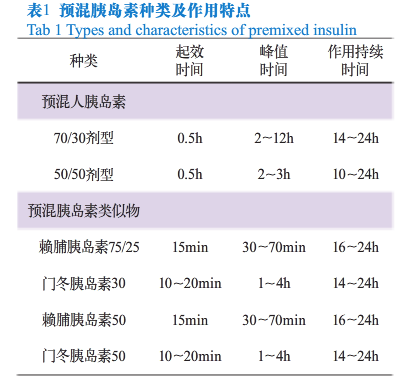
预混人胰岛素:预混人胰岛素是指将重组人胰岛素(短效)与精蛋白锌重组人胰岛素(中效)按一定比例混合而成的胰岛素制剂,包括低预混人胰岛素和中预混人胰岛素。
预混胰岛素类似物:预混胰岛素类似物是指将速效胰岛素类似物(赖脯胰岛素或门冬胰岛素)与精蛋白锌速效胰岛素类似物按一定比例混合而成的胰岛素制剂,包括低预混胰岛素类似物和中预混胰岛素类似物。
2、预混胰岛素治疗方案
2.1 每日1次方案
(1)适用人群:生活方式干预及两种或两种以上口服降糖药最大有效剂量治疗后HbA1c≥7.0%的患者。
(2)预混胰岛素选择:低预混人胰岛素、低预混胰岛素类似物、中预混人胰岛素、中预混胰岛素类似物。
(3)起始剂量:每日1次起始剂量一般为0.2IU/(kg•d),晚餐前注射,根据患者情况作适当调整。
(4)注意事项:
①如果HbA1c或空腹血糖仍不达标,则可改为每日2次治疗方案,可参考1-2-3次方案;
②预混人胰岛素应在餐前30min皮下注射,预混胰岛素类似物可在餐前即刻注射或餐后即注射;
③在预混胰岛素选择方面,临床医生应注意根据患者具体情况决定,中预混胰岛素主要针对餐后血糖升高明显的患者;
④可根据患者具体情况调整口服降糖药。
2.2 每日2次方案
(1)适用人群:
①新诊断T2DM患者,HbA1c≥9.0%同时合并明显临床症状;
②生活方式干预及两种或两种以上口服降糖药最大有效剂量治疗后HbA1c≥9.0%的患者;
③口服降糖药物联合基础胰岛素治疗以后,HbA1c≥7%,而空腹血糖已达标的患者。
(2)预混胰岛素选择: 低预混人胰岛素、低预混胰岛素类似物、中预混人胰岛素、中预混胰岛素类似物。
(3)起始剂量:对于①、②患者的情况,一般为0.2~0.4IU/(kg•d)或10~12IU/d,按1:1分配到早餐前和晚餐前;对于③患者的情况,一般以基础胰岛素与预混胰岛素以1:1.3的比例进行剂量转换,按1:1分配到早餐前和晚餐前。临床医生一定要根据患者具体情况决定预混胰岛素类别、日总剂量和早晚餐前剂量的分配。
(4)注意事项:
①采用预混胰岛素每日2次治疗方案时,不建议同时使用胰岛素促泌剂(主要不良反应与胰岛素一致,为低血糖和体重增加);
②可继续使用二甲双胍或α-糖苷酶抑制剂,视患者个体情况决定是否停用TZD类药物;
③按时、定量进餐及规律运动,预混人胰岛素应在早、晚餐前30min皮下注射,预混胰岛素类似物可在餐前即刻注射或餐后立即注射;
④中预混胰岛素主要针对餐后血糖升高明显或者血糖波动较大的患者(如口服降糖药失效后,早餐后血糖≥13.5mmol/L或早餐前后血糖波动≥4.4mmol/L),以及饮食中碳水化合物比例较高的患者;
⑤若低预混人胰岛素每日2次治疗的患者餐后血糖≥11.1mmol/L,临床医生可依据具体情况考虑等剂量改为低预混胰岛素类似物或中预混胰岛素类似物。
2.3 每日3次方案
(1)适用人群:
①预混胰岛素每日2次治疗后HbA1c≥7.0%的患者。
②血糖控制不达标,需要基础+餐时胰岛素强化治疗,但不愿意接受该治疗方案的患者。
(2)预混胰岛素选择:低预混胰岛素类似物、中预混胰岛素类似物。
(3)起始剂量:对于①患者的情况,早晚餐前等剂量转换,午餐前加2~4IU或每天胰岛素总量的10%,并可能需要减少早餐前的剂量2~4IU;对于②患者的情况,临床医生根据具体情况决定。
(4)注意事项:
①如果预混胰岛素从每日2次增加至每日3次时,建议将预混人胰岛素改为预混胰岛素类似物;
②若低预混胰岛素每日2次治疗,HbA1c≥7.0%,早餐后血糖<10.0mmol/L,可考虑调整为低预混胰岛素类似物每日3次;若早餐后血糖≥10.0mmol/L的患者,则可考虑调整为中预混胰岛素类似物每日3次治疗;
③预混胰岛素类似物可在餐前即刻注射或餐后立即注射;
④对于中预混胰岛素类似物每日3次治疗患者,如果餐后血糖控制好而空腹血糖>6mmol/L时,可考虑将晚餐前调整为低预混胰岛素类似物。
2.4 1-2-3次方案
1-2-3次方案是指,对于采用生活方式干预及两种或两种以上口服降糖药最大有效剂量治疗血糖仍不达标(HbA1c≥7.0%)的患者,起始每日1次预混胰岛素类似物注射,血糖控制仍不达标时,可逐渐增加到每日2次、每日3次的方案。
(1)适用人群:生活方式干预及两种或两种以上口服降糖药最大有效剂量治疗后HbA1c≥7.0%的患者。
(2)预混胰岛素选择:低预混胰岛素类似物、中预混胰岛素类似物。
(3)起始剂量:预混胰岛素类似物每日1次起始剂量一般为10~12IU,晚餐前注射,根据早餐前血糖调整剂量;如果治疗后HbA1c或餐前血糖不达标,则早餐前加用预混胰岛素类似物3~6IU,根据晚餐前和空腹血糖调整早餐前和晚餐前剂量;如果治疗后HbA1c或午餐后血糖不达标,则午餐前加用预混胰岛素类似物3IU或将早餐前剂量按1:1分配到早、午餐前,根据午餐后或晚餐前血糖调整午餐前剂量。
(4)注意事项:
①一般在口服降糖药治疗的基础上加用预混胰岛素类似物每日1次治疗,临床医生也可根据患者具体情况调整口服降糖药;
②当调整为预混胰岛素类似物每日2次或每日3次治疗时,不建议同时使用胰岛素促泌剂(主要不良反应与胰岛素一致,为低血糖和体重增加);
③可继续使用二甲双胍或α-糖苷酶抑制剂,视患者个体情况决定是否停用TZD类药物;
④中预混胰岛素类似物主要针对餐后血糖升高明显的患者;
⑤预混胰岛素类似物应在餐前即刻注射或餐后立即注射。
3、自我血糖监测
自我血糖监测(self-monitoring of blood glucose,SMBG)是糖尿病管理中的重要组成部分,其结果有助于评估降糖治疗的效果并指导治疗方案的调整。可根据不同的胰岛素治疗方案制定个体化的SMBG方案。
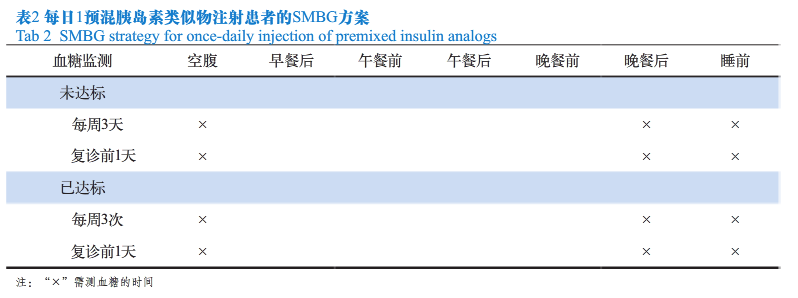
3.1 每日1次预混胰岛素类似物治疗的SMBG方案
每日1次预混胰岛素类似物治疗的患者在血糖达标前每周监测3天空腹、晚餐后和睡前血糖,每2周复诊1次,复诊前1天加测3个时间点血糖;在血糖达标后每周监测3次血糖,即空腹、晚餐后和睡前血糖,每月复诊1次,复诊前1天加测3个时间点血糖(见表2)。
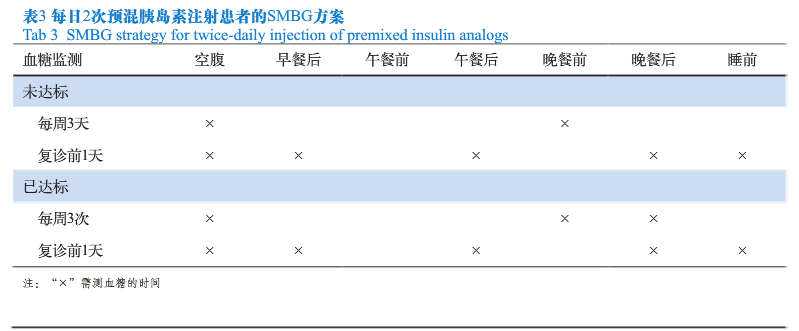
3.2 每日2次预混胰岛素(包括预混人胰岛素和预混胰岛素类似物)治疗的SMBG方案
每日2次预混胰岛素治疗的患者在血糖达标前每周监测3天空腹和晚餐前血糖,每2周复诊1次,复诊前1天加测5个时间点血糖;在血糖达标后每周监测3次血糖,即空腹、晚餐前和晚餐后血糖,每月复诊1次,复诊前1天加测5个时间点血糖(见表3)。
3.3 每日3次预混胰岛素类似物治疗的SMBG方案
每日3次预混胰岛素类似物治疗的开始阶段应每天监测5~7个时间点血糖,包括空腹、三餐前后、睡前,血糖达标后每日监测2~4个时间点血糖(见表4)。

3.4 注意事项 :
在胰岛素治疗期间,如有低血糖表现时需随时监测血糖;如出现不可解释的空腹高血糖或夜间低血糖时,应监测夜间血糖(如3am血糖)。
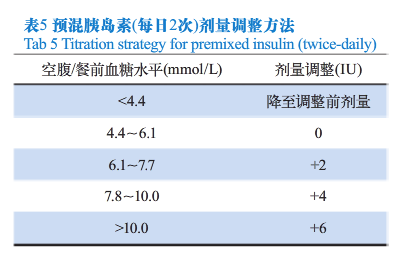
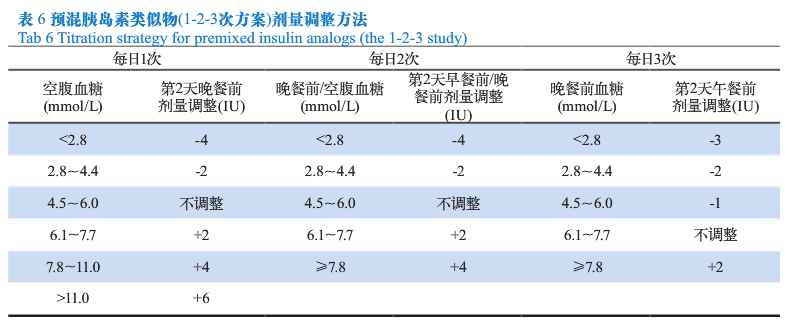
4、预混胰岛素剂量调整方法
临床医生应根据患者具体情况设定血糖控制目标。在胰岛素治疗期间,结合血糖监测结果,适时调整治疗方案和胰岛素剂量,以取得良好的血糖控制。对于不同的预混胰岛素治疗方案,其剂量调整方法有所不同,可参考每日2次预混胰岛素治疗方案(见表5)和1-2-3次预混胰岛素类似物治疗方案的剂量调整方法(见表6),每3~5天调整1次,每次调整1~4IU,直至血糖达标。
5、需要注意的情况
T2DM患者的血糖控制目标因患者的年龄、合并症、并发症等不同而异,临床医生应注意结合患者病情、经济等各方面的因素综合考虑,选择适合患者的治疗方案。对已合并心脑血管疾病或其他危险因素的T2DM患者,在胰岛素治疗治疗时,应当采取稳妥、安全的降糖治疗措施和目标值,尽量避免低血糖的发生。
6、总结
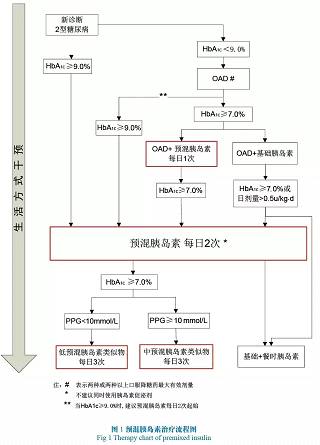
预混胰岛素能同时提供基础及餐时胰岛素,方案简便、易操作,在中国糖尿病患者中应用广泛。临床医生要根据患者的具体情况综合考虑,包括生活方式、方案的简便程度,长期依从性,血糖监测及低血糖发生等多种因素,制定个体化的胰岛素治疗方案。预混胰岛素基本治疗路线(见图1)的制定借鉴了国内外诸多临床研究的经验,为实际应用提供指导和帮助。
来源:中华医学会内分泌学分会.预混胰岛素临床应用专家共识(2016年版).药品评价.2016,13(9):5-11.)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#临床应用#
28
#专家共识#
30
#胰岛#
18
文章很好,非常有益
73
学习学习。。。
70
继续学习
59
继续关注
60
继续学习
47
继续关注
29
很好的课程,学到很多,继续学习
23