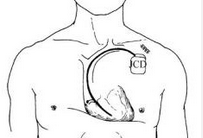
AIM:植入式心律转复除颤器植入后长期风险增加
2016-05-07 崔倩 译 MedSci原创
植入式心律转复除颤器(ICD)植入后长期非致命性结果还没有被定义。该研究的目的是确定与ICD相关并发症需要再次手术或住院的长期风险,以及除并发症之外的原因再次手术的风险,并评估相关的患者和设备的特性。来自美国的研究人员进行了一项ICD移植的观察性队列研究,这些ICD移植数据来自于国家心血管数据注册ICD登记医疗有偿服务索赔数据。该研究在1437家美国医院进行,共包括114484名65岁及以上的患者
植入式心律转复除颤器(ICD)植入后长期非致命性结果还没有被定义。
该研究的目的是确定与ICD相关并发症需要再次手术或住院的长期风险,以及除并发症之外的原因再次手术的风险,并评估相关的患者和设备的特性。
来自美国的研究人员进行了一项ICD移植的观察性队列研究,这些ICD移植数据来自于国家心血管数据注册ICD登记医疗有偿服务索赔数据。
该研究在1437家美国医院进行,共包括114484名65岁及以上的患者(平均74.8岁[SD,6.2];72.4%为男性),这些患者在2006年到2010年间首次接受ICD移植(单腔,19.8%;双腔,41.3%;心脏再同步除颤器[CRT-D],38.9%)。
主要检测指标为因ICD相关并发症需要再次手术或住院治疗,以及除并发症之外原因再次手术的累计发生率。
在平均随访2.7年中(四分位距,1.8至3.9年),40072例患者死亡,每100名患者年的随访死亡率为12.6(95%CI,12.5〜12.7)。因为ICD相关并发症需要再次手术或住院的每100患者年中,死亡风险为6.1(CI,6.0〜6.2),因为其他原因需要再次手术的每100患者年中,死亡风险为3.9(CI,3.8〜4.0)。总体而言,每100患者年的随访过程就有10例患者有并发症或再次手术的风险。植入时年龄偏小(65至69 vs >85岁)(危险比[HR],1.55[CI,1.43〜1.69]),接受CRT-D装置(HR,1.38[CI,1.31〜1.45])vs 单腔装置,女性(HR,1.16[CI,1.12至1.21]),和黑色人种(HR,1.14[CI,1.05〜1.23)均与ICD相关并发症的最大风险增加有关。
该研究的限制性为数据只分析了65岁及以上的人群。
ICD移植后,患者的设置相关并发症发生率和其他原因再次手术发生率都增加了。ICD植入风险和减少这些风险的策略都是应该在植入之前需要考虑到的。
原始出处:
Isuru Ranasinghe,Craig S. Parzynski,James V. Freeman,et al.Long-Term Risk for Device-Related Complications and Reoperations After Implantable Cardioverter-Defibrillator Implantation,AIM.2016.5.3
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#心律转复除颤器#
32
#植入式#
25
#长期风险#
28
#植入式心律转复除颤器#
33
#除颤#
42
#植入#
32