关于锶-89治疗肿瘤骨转移,所有你想知道的都在这里!
2018-05-30 佚名 中国核学会核医学分会科普教育委员会
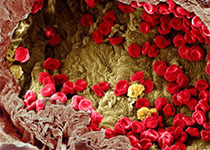
癌症骨转移是恶性肿瘤常见的并发症之一,约65%~80%的恶性肿瘤晚期会发生骨转移,其发病率约为原发恶性骨肿瘤的35~40倍,好发于中老年,男女比例约为3:1。
癌症骨转移是恶性肿瘤常见的并发症之一,约65%~80%的恶性肿瘤晚期会发生骨转移,其发病率约为原发恶性骨肿瘤的35~40倍,好发于中老年,男女比例约为3:1。
一、骨转移癌及骨痛会给患者造成哪些不良影响?
由骨转移癌引起的相关骨事件包括骨痛 50%~90%、病理性骨折5%~40%、高钙血症10%~20%、脊柱不稳和脊髓神经根压迫症状<10%和骨髓抑制<10%。
其中,骨痛发生率最高,多为顽固性、持续性的剧烈疼痛,患者会感到极度不适,引起或加重患者的焦虑、抑郁、乏力、失眠、食欲减退等症状,严重影响患者的日常活动、自理能力、交往能力及整体生活质量。相关的综合治疗费用,也会增加患者的经济负担。
二、骨转移癌及骨痛目前有哪些治疗方法?
骨转移癌属于晚期病变,以姑息治疗为主,治疗目标包括3 个方面:缓解疼痛,恢复功能,改善生活质量;预防和治疗骨相关事件;控制肿瘤进展,延长生存期。
临床上,针对骨转移癌及骨痛的治疗多采用综合性治疗,包括:手术、放疗(外放射治疗)、化疗、药物(双膦酸盐、止痛药、激素及中医中药等)、营养支持治疗和放射性核素治疗。
外科手术主要目的是防止和治疗病理性骨折;
放疗适用于单发病灶,可有效缓解骨痛,控制局部病变的发展,但在多发性骨转移癌患者应用受限;
化疗的疗效取决于肿瘤对化疗药物的敏感程度,全身不良反应较多,患者往往难以耐受;
双磷酸盐类药物治疗主要是通过抑制破骨细胞的活性,进而阻断病理性溶骨,可预防或延缓骨相关事件的发生,但不能直接杀死肿瘤细胞;
止痛药物能在一定程度上缓解患者的疼痛,但对骨转移灶本身无治疗作用,且长期使用不良反应多。
放射性核素治疗主要用于广泛性骨转移癌患者,已有50多年的历史,可以特异性杀死骨转移肿瘤细胞,从而发挥持久的镇痛作用。
锶-89在英国80年代开始正式应用于临床,90年代获美国FDA批准。具有给药剂量低、毒副作用小、疗效维持时间长等特点,目前临床应用更广泛。
三、锶-89为什么能用来治疗骨转移癌和骨转移癌所致的骨痛?
锶-89治疗骨转移癌的原理:锶-89进入体内后,可选择性浓聚于骨代谢异常活跃的骨肿瘤病灶部位,病灶对锶-89的摄取是正常骨的2~25倍,其释放出的β射线对肿瘤细胞具有集中、持久、直接杀伤作用。
锶-89治疗镇痛原理:
1、辐射作用使肿瘤体积缩小,减轻了受累骨膜和骨髓腔的压力;
2、辐射作用杀死肿瘤细胞,使扩散到神经组织导致疼痛的肿瘤细胞数量减少;
3、辐射生物效应抑制缓激肽和前列腺素等疼痛介质的产生;
4、辐射生物学效应干扰神经末稍去极化的过程,影响了疼痛信号在轴索的传导;
5降低碱性磷酸酶和前列腺素水平,减轻骨质破坏,从而减少对骨膜中痛觉纤维的刺激。
四、哪些人适合锶-89治疗(适应症)?
1、骨转移癌伴有骨痛患者,且骨显像显示有放射性浓聚;
2、恶性骨肿瘤因种种原因未能手术切除或手术后有残留癌肿,且骨显像证实有较高的放射性浓聚;
3、白细胞不低于3.5×109/L,血小板不低于80×109/L。
五、哪些人不适合锶-89治疗(禁忌症)?
1、6周内进行过化疗;
2、化疗或放疗后出现严重骨髓功能障碍;
3、骨显像显示病灶无明显放射性浓聚,呈放射性“冷区”的溶骨性病变;
4、严重肝肾功能损害者;
5、妊娠和哺乳期妇女;
6、对于由于脊柱转移引起的脊索压迫,可能需要更快速的治疗,锶-89不能作为主要治疗手段。
六、锶-89治疗骨转移癌及骨痛的疗效如何?
锶-89半衰期长(50.5天),可以在骨转移癌病灶内滞留约100天,因此疗效持久。
疗效主要体现在骨痛的缓解,改善患者的生活质量、预防或减少骨相关事件的发生,部分患者骨转移病灶可有不同程度的缩小甚至消失。
临床研究显示,多数患者在治疗后2周疼痛逐渐缓解,有效率在80%以上,且疼痛缓解维持时间3~6个月。
七、锶-89治疗骨转移癌及骨痛安全吗?
锶-89治疗骨转移癌及骨痛不仅有效,并且安全。锶-89治疗后毒副作用包括早期副作用和后期副作用。
早期副作用发生在治疗后2~10天,少数患者可出现骨痛加剧,即所谓的“闪烁”现象或称之为“反跳痛”,一般持续2~4天。
“闪烁”现象的发生机制尚不明确,但出现“闪烁”现象的患者常预示将获得较好的疗效。
后期副作用主要是短暂性骨髓抑制,表现为治疗后4~6周约20%~30%的患者会出现一过性白细胞和(或)血小板降低,下降幅度较治疗前基础值一般小于20%,对症处理即可。罕见不可逆性骨髓抑制。
八、锶-89治疗后辐射危害大吗?
锶-89发射纯β射线,平均能量约1.5 Mev,射程短(骨组织中的最大射程约3毫米,软组织中约8毫米),穿透力差,1厘米厚的木板可将其大部分屏蔽,因此对患者家属、周围环境和医护人员的辐射危害可忽略不计,无需进行特殊的辐射防护。
另一方面,锶-89具有趋骨性,靶向性强,故患者本身除骨转移病灶以外的组织和器官辐射剂量极小。
九、可否重复治疗?
可以。但需遵循以下指征:
1、骨痛未完全消失或有复发者;
2、首次治疗效果明显,白细胞>3.5×109/L,血小板>80×109/L;
3、两次治疗时间应间隔3个月以上。
十、可否与其他治疗方法并用?
可以。研究显示,锶-89与放疗、化疗、双膦酸盐及内分泌治疗等联合治疗具有协同效应,效果更好,安全性也较高。
值得注意的是,联合治疗时需把控好两种不同治疗方法的间隔时间,如锶-89治疗前应停用化疗或放疗至少6周避免发生骨髓抑制,停用双膦酸盐药物至少2天以利于锶-89在骨转移病灶中积聚。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#锶#
33
谢谢分享.学习了
54
阅
55
学习了.长知识
60
学习了
68