Phytomedicine:丹芪通脉片复扰氧脂素以减轻急性心肌梗死
2022-04-25 紫菀款冬 MedSci原创
探究丹芪通脉片对急性心肌梗死的作用靶点和机制。

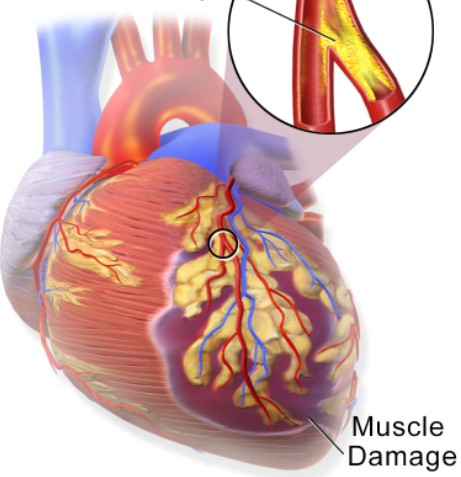
背景:急性心肌梗死(AMI)已成为全球发病率和死亡率增加的主要原因之一,AMI的缺血后炎症反应决定了缺血心脏修复和瘢痕形成的路径,丹芪通脉片(DQTT)临床常治疗AMI,其中丹酚酸(SA)与三七皂苷(PNE)是DQTT主要活性物质,其大部分成分具有抗炎活性,特别是当它们在体内吸收时,然而DQTT在治疗AMI机制上对氧脂素代谢的调控机制尚未建立。
目的:探究DQTT对AMI的作用靶点和机制。
方法:通过网络药理学对主要成分SA和PNE进行靶点预测——花生四烯酸通路可能参与了DQTT对AMI的治疗作用。
建立H9C2心肌细胞的氧-糖剥夺/再氧模型验证花生四烯酸通路对环氧化酶(COX)和脂氧合酶(LOX)的调控作用。
动物实验中将大鼠随机分为7组:假手术组、AMI组、DQTT (65 mg/kg)、DQTT (130 mg/kg)、DQTT (260 mg/kg)、SA (22 mg/kg)、PNE (108 mg/kg),每组10只。采用LC/MS/ MS法对AMI大鼠进行DQTT氧磷脂靶向治疗。采用超高效液相色谱-三重四极杆质谱(UHPLC-QqQ/MS)检测系统测定AMI大鼠血浆38种氧磷脂的浓度。
使用细胞因子阵列,探究DQTT的抗炎作用显示为显著下调促炎细胞因子。
通过基因验证COX和LOX的表达和蛋白水平,验证恢复被干扰的花生四烯酸代谢是DQTT治疗AMI炎症的主要机制。
结果:细胞及动物实验发现通过DQTT治疗,受干扰的花生四烯酸代谢组部分恢复,抗炎脂蛋白显著升高,促炎脂蛋白降低。DQTT通过花生四烯酸代谢、嘌呤代谢以及丙氨酸、天冬氨酸和谷氨酸代谢等多种代谢途径恢复AMI大鼠的稳态。细胞因子阵列分析发现,DQTT通过下调缺血心肌组织中COX-2和ALOX5,使促炎细胞因子显著下调。
结论:DQTT可有效治疗急性心肌梗死,受干扰的花生四烯酸代谢组部分以剂量依赖性的方式得以恢复,抗炎代谢物显著升高,促炎脂质降低,证实DQTT对缺血组织损伤的抗炎作用。该研究表明,DQTT可能是一种很有前景的治疗AMI药物。
文献来源:Zhi H, Zhang Z, Deng Y, etal. Restoring perturbed oxylipins with Danqi Tongmai Tablet attenuates acute myocardial infarction. Phytomedicine. 2021 Sep;90:153616.doi:10.1016/j.phymed.2021.153616
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#DIC#
50
#CIN#
34
#Medicine#
38
#Med#
0