2017 版NCCN结直肠癌指南更新,左右半结肠癌之争终入指南
2016-12-14 中山大学肿瘤医院结直肠科 陈功 医师报
11月23日,美国国立综合癌症网络(NCCN)在线发布了2017版结肠癌和直肠癌临床实践指南,和2016年V2版对比,出现了很多能改变临床实践的更新。其中,尤以左右半结肠癌的问题备受关注。指南推荐将原发瘤部位纳入转移性结直肠癌(mCRC)一线治疗中靶向药物的选择参考依据,这必将是里程碑式的更新,也将是引起轩然大波的更新。更新一:RAS野生型mCRC一线靶向治疗的推荐,EGFR单抗(西妥昔单抗和
11月23日,美国国立综合癌症网络(NCCN)在线发布了2017版结肠癌和直肠癌临床实践指南,和2016年V2版对比,出现了很多能改变临床实践的更新。其中,尤以左右半结肠癌的问题备受关注。指南推荐将原发瘤部位纳入转移性结直肠癌(mCRC)一线治疗中靶向药物的选择参考依据,这必将是里程碑式的更新,也将是引起轩然大波的更新。
更新一:RAS野生型mCRC一线靶向治疗的推荐,EGFR单抗(西妥昔单抗和帕尼单抗)仅限于左侧结肠癌患者。
情理之中
关于原发瘤部位在mCRC治疗决策中的作用,也就是热门话题“左右半之争”。首先已明确的观点是,肿瘤部位是Ⅲ/Ⅳ期结直肠癌独立的预后因素,右半结肠癌预后显著差于左半结肠和直肠,与治疗手段无关。其次,原发瘤部位是EGFR靶向治疗的负性疗效预测指标。
回顾性数据表明,贝伐单抗(Bev)在mCRC的疗效也许与原发肿瘤部位没有关系,其在左、右半肿瘤中的获益均是稳定的。但抗EGFR靶向治疗的疗效和部位存在很明显的关系,在左半结肠中,抗EGFR均能带来显著获益;反之,右半结肠的获益则明显减少或不能获益;贝伐单抗在右半的获益显著高于抗EGFR靶向治疗。因此,即使RAS野生型的右半结肠癌,也不能从抗EGFR治疗中获益或获益明显减少。
那么,原发瘤部位背后是否还隐藏着一条或多条目前尚未发现的、独立于RAS/RAF通路的、对EGFR靶向治疗耐药的分子同道呢?在没有完全明确前,或可将原发瘤部位作为抗EGFR单抗的替代负性疗效预测标志物。指南的更新呼应了上述发现与假说,而终将“左右半之争”纳入指南。
指南更新的内容,仅针对右侧mCRC来限定了抗EGFR靶向药物的使用,却没对左侧mCRC的靶向选择给出倾向性建议,这将是最有争议之处。
争议一
EGFR单抗不能用于右侧mCRC的治疗吗?
首先,“仅限于右侧肿瘤”中的限定仅用于一线治疗,在二线及后续治疗中,对EGFR单抗的使用是没有限制原发瘤部位的。也就是说, RAS野生型右半mCRC在二线以后还是可以使用EGFR单抗的。
其次,指南中对于mCRC的一线推荐,其基本常识就是化疗+靶向是mCRC的标准治疗模式。换而言之,这种推荐是基于将“化疗+Bev”来作为基准对照后给出的,对于和单纯化疗相比的情况,数据是很不充分的。
争议二
回顾性数据可见,在左侧mCRC中,不管是和单纯化疗相比,还是和Bev相比,EGFR单抗都显示出显著的生存获益。那么,指南为何对于左侧肿瘤,不优先推荐EGFR单抗呢?
FIRE-3研究表明,右侧肿瘤中Bev对于西妥昔单抗(Cet)的相对获益大于左侧。而考虑到Bev是美国医保的标准治疗药物、耐受性更好等客观因素,指南将这两个靶向药物做同级别推荐就不足为奇了。
笔者认为,应优先推荐Cet用于左侧mCRC的治疗,并综合考虑毒性、患者意愿、治疗花费等因素。
更新二:初始可切除mCRC的肝/肺转移瘤的新辅助化疗方案中,删除了靶向药物。
2016年是戏剧性的一年,关于“初始可切除mCRC新辅助治疗是否应该使用靶向药物”这个热门话题,国际两大主流指南ESMO和NCCN,一个向左,一个向右,分歧再起。
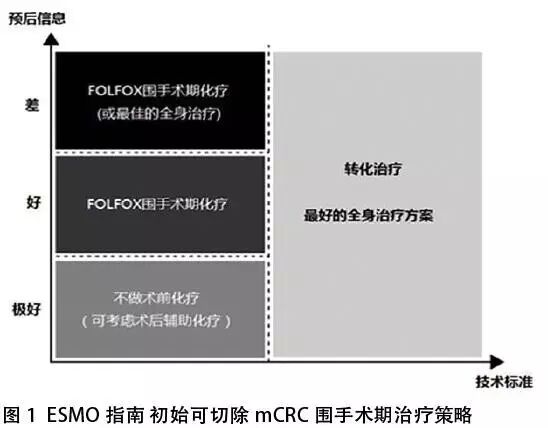
2015-2016年,ESMO指南在初始可切除mCRC围手术期的治疗模式中,做了较大更改。明确提出要从“手术技术标准”和“肿瘤学预后因素”两个维度进行考量(图1)。笔者认为,ESMO 2015/2016指南的发布,给肿瘤内科医师去掉了一直以来的“紧箍咒”。然而,当我们认为ESMO和NCCN渐趋一致的时候,2017NCCN指南却做出相反的更新。
该问题的核心是“可切除”的标准。然而,临床研究和临床实践使用的标准并不统一。迄今为止,所有以“手术切除”为主要目标的临床随机对照研究,均把“可切除肝转移定义为“数目<5个”。事实上,在临床实践或NCCN指南中,讨论的“可切除”往往指单纯技术上的可切除,没有考虑肿瘤学的因素,这显然是不合理的。
因此,笔者不赞同NCCN指南中对新辅助化疗中完全删除靶向药物的更新。强烈建议采纳ESMO指南的观点,一定要从“技术标准”和“预后信息”两个维度来参考决策,对于预后差的技术上“可切除”mCRC,术前新辅助治疗不该排除靶向药物。
更新三:早期结直肠癌(CRC)患者根治术后,推荐口服低剂量阿司匹林作为二级化学预防。
近年,既往研究主要关注阿司匹林在结直肠癌化学预防领域的两大作用:减少健康人群中CRC的发生率(一级预防);减少罹患CRC者根治术后的肿瘤复发(二级预防)。
阿司匹林对结直肠癌二级预防的价值,最著名的证据来自哈佛大学麻省总院陈志辉团队的发现。研究显示,阿司匹林对结肠癌术后复发的预防,可能与PIK3CA基因突变有关。
荷兰莱登大学医学院研究表明,除胰腺癌外,其他消化道肿瘤患者均从阿司匹林中获益,其中结直肠癌患者获益最大。
新加坡国立癌症中心的ASCOLT研究,是该领域中最受关注的随机对照试验(RCT)之一。该研究针对接受四个月以上氟脲嘧啶为基础的辅助化疗(放疗不限)的Ⅱ/Ⅲ期结直肠癌患者。标准治疗结束后,随机接受阿司匹林200 mg/d或安慰剂治疗,共3年。该研究拟入组超过1000例患者,笔者所在中心也参与了ASCOLT研究。期待这个研究能进一步解答阿司匹林在结直肠癌防治中的价值。
前瞻性RCT的结果尚未问世,新指南里已做推荐,这是很不寻常的。但也在一定程度上体现了业界对该问题看法的一致性。小小的百年神药阿司匹林,能否在结直肠癌防治中发挥大大的作用?我们拭目以待。
更新四:首次推荐PD-1单抗免疫治疗用于具有dMMR/MSI-H分子表型的mCRC的末线治疗。
2015年迎来了突破性进展,ASCO会议上公布了一项研究,该研究首次通过错配修复(MMR)基因状态,筛选出富集了对程序性死亡受体(抗PD-1)免疫治疗有效的mCRC。次年该研究扩大了dMMR CRC组样本数,结果仍然一致。
NCCN基于此做出指南更新似乎迟了些。该研究的重要性在于,其不但为正陷于治疗困境中的mCRC带来了突破性进展,还开启了免疫治疗的新思路——基于基因/标志物富集的“精准”免疫治疗。
众所周知,不是所有癌症、某一癌症的所有患者均对免疫治疗有效,如何富集有效人群,是临床所面临的问题。尽管dMMR CRC免疫治疗取得了突破性进展,但是dMMR肿瘤的比例是极少的。对于高比例的pMMR患者,如何提高疗效,寻找其他的疗效预测标志物,仍是个艰巨的任务。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#指南更新#
33
很好,不错,以后会多学习
89
文章好好
59
很好,不错,以后会多学习
0
继续努力
72
#NCCN#
23
#结直肠#
20
指南就是方向
64
指南
17
很好,不错的指南资料,值得拥有值得收藏,值得探究。给自己学习探究提供方便。点个赞!
22