Injury:桡骨远端骨折合并桡动脉损伤动脉修复效果良好
2013-05-29 Injury 丁香园
桡骨远端骨折合并桡动脉损伤在临床中较为少见,通常被认为是高能量损伤导致的一种少见的损伤,目前并没有单独报道两者合并损伤的文献资料,较难得出其具体发病率。因目前文献资料较少,很难对桡骨远段合并桡动脉损伤患者的临床特征和功能预后进行判断。近日来自美国Maryland大学医学院的学者进行了一项研究,针对其所在的一级创伤治疗中心数十例桡骨远端骨折合并桡动脉损伤的患者进行手术修复,对功能预后情况进行总结,相
桡骨远端骨折合并桡动脉损伤在临床中较为少见,通常被认为是高能量损伤导致的一种少见的损伤,目前并没有单独报道两者合并损伤的文献资料,较难得出其具体发病率。因目前文献资料较少,很难对桡骨远段合并桡动脉损伤患者的临床特征和功能预后进行判断。近日来自美国Maryland大学医学院的学者进行了一项研究,针对其所在的一级创伤治疗中心数十例桡骨远端骨折合并桡动脉损伤的患者进行手术修复,对功能预后情况进行总结,相关结论发表在injury上。
研究组共包括1999年-2004年5年间14例桡骨远端骨折合并桡动脉损伤的患者,其中9例患者动脉损伤为溃疡性,5例患者为血栓栓塞性;对照组患者共包括2003年-2005年3年间380例桡骨远端骨折行掌侧入路内固定的患者。所有患者均接受同一医生手术治疗。
手术方法:掌侧入路,直视下暴露桡动脉,观察桡动脉的完整和通畅性。取桡侧腕屈肌和桡动脉间入路,该入路可避免经腕屈肌腱鞘暴露造成的后期该部位疤痕形成和术后肢体僵硬。若患者骨折复位困难,需要行背侧固定时,追加背侧入路。桡骨骨折按常规固定方法进行。对所有动脉损伤为溃疡性损伤的患者,清创处理两个断端,修建断端血管,直至正常管腔;对血栓性损伤的患者,在栓塞远端横断切开桡动脉,使用Fogarty导管清除血栓,切除损伤动脉端至正常管腔。使用8/0尼龙线进行端端吻合。吻合完成后使用多普勒超声仪对血流情况进行检测。术后不使用抗凝药物。
患者术后随访时间点为2周,6周,12周及骨折愈合时,共12/14(86%)例患者完成随访,平均随访时间52周。
使用临床评分表评估患者的腕关节运动度及恢复原先工作能力;使用Doppler Allen试验评估患者的桡动脉通畅水平;收集患者骨折类型,年龄,ISS评分,GCS评分,休克指数,住院时间等,并将试验组和对照组进行比较。
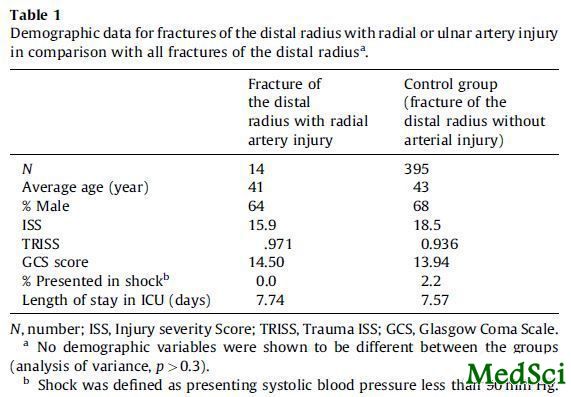
研究结果如表1所示。
表1:试验组和对照组相关统计数据比较
对需要行掌侧入路手术治疗的桡骨远端骨折患者,合并桡动脉损伤的概率是2%(14/5=2.8,380/3=127,2.8/127=2%)。
两组患者术前ISS评分,平均住院日等指标无显著差异,提示桡骨远端骨折合并桡动脉损伤患者的术前损伤可能并不是因为高能量暴力所至。
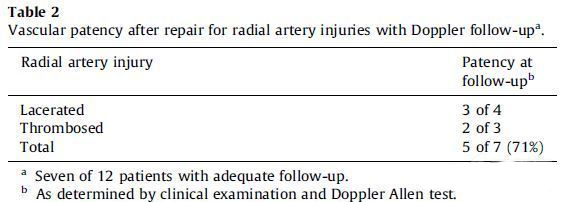
在12例完成随访的患者中,共7例患者进行了桡动脉的Allen试验检查,5例患者桡动脉通畅,总体通畅率71%,其中溃疡组2/3例,血栓组3/4例,如表2所示。
表2:随访过程中患者桡动脉血管的再通率
随访结束时患者腕关节运动度:屈曲39度,伸直40度,旋前69度,旋后65度;没有患者出现手腕部位不能耐受寒冷症状;7/12例患者存在持续的腕关节不适感,但临床症状并非源于神经或血管方面;只有3/12例患者最后返回至原先工作岗位,但其他不能返回原先工作岗位的患者原因是合并有其他损伤而并非腕关节部位损伤。
研究者最后进行了总结:对需要行掌侧入路手术治疗的桡骨远端骨折患者,合并桡动脉损伤的概率约为2%; 14例患者有9例患者为开放性骨折,参照以往的文献,提示开放性桡骨远端骨折可能是桡动脉损伤的一个重要的危险因子;试验组与对照组在损伤严重评分上相类似提示桡骨骨折合并桡动脉损伤和单纯桡骨远端骨折的暴力相类似;既往文献报道,桡动脉损伤修复后的再通率约55%(表3),本试验桡动脉再通率可达到70%左右,但若考虑到失随访患者数,和既往文献报道相当,证实桡动脉再通率较低;尽管如此,桡动脉堵塞患者患肢无明显缺血症状,因此后期需要更多的对桡动脉修复后患者腕部功能是否得到改善的研究进行明确。
表3:以往对桡动脉损伤修复后血管再通率的报道
Fracture of the distal radius with radial artery injury: injury description and outcome of vascular repair.
INTRODUCTION
The ideal treatment of an isolated radial artery injury that is associated with a fracture of the distal radius is unknown. Our purposes were to assess the incidence of this injury pattern and to describe the outcomes of our treatment protocol. We hypothesised that combined routine repair of the artery during operative treatment results in a satisfactory outcome.
METHODS
Our study group consisted of 14 patients who were treated by one surgeon with a consistent treatment algorithm. The average follow-up duration was 52 weeks. Our control group consisted of 380 patients with fracture of the distal radius without radial artery injury, who were treated by the same surgeon during a 3-year period.
RESULTS
We observed a 2% incidence of isolated radial artery injury in patients treated with open reduction and internal fixation (ORIF) of the distal radius. Outcomes were comparable to those reported for operative treatment of fractures of the distal radius without radial artery injury.
CONCLUSIONS
Our protocol resulted in adequate outcomes, a 71% patency rate (five of seven fractures with adequate vascular follow-up) and no evidence of symptoms related to a poorly perfused hand.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Injury#
40
#动脉损伤#
34
#损伤#
42
#桡动脉#
45
#桡骨远端骨折#
57
#桡骨#
40