Cardiovasc Diabetol:SGLT2抑制剂在糖尿病合并心力衰竭患者中的当代应用情况
2022-08-18 MedSci原创 MedSci原创
使用 SGLT2 抑制剂与超老龄社会中广泛的 HF 合并 DM 患者的一年死亡率和 HF 再入院风险降低相关。
糖尿病 (DM) 是发展为心力衰竭 (HF) 的重要危险因素。与非糖尿病患者相比,糖尿病的者因心力衰竭而需要住院的风险高出 30%。钠-葡萄糖协同转运蛋白 2 抑制剂 (SGLT2-I) 可显著降低心衰住院率以及心血管和肾脏不良结局风险。
该研究采用日本全国健康数据库调查了在超老龄社会广泛的 HF 合并 DM 的住院患者中使用 SGLT2 抑制剂与一年预后之间的相关性。
研究人员从日本国家健康保险索赔和特定健康检查数据库中检索从2014 年 4 月-2019 年 3 月期间登记的首次急性心衰住院患者,分成了两个队列,SGLT2 抑制剂使用者(n=2277)和二肽基肽酶 4 (DPP4) 抑制剂使用者(n=41410),将两个队列进行了对比。并对两个队列各2101位受试患者进行了倾向得分匹配的队列研究。
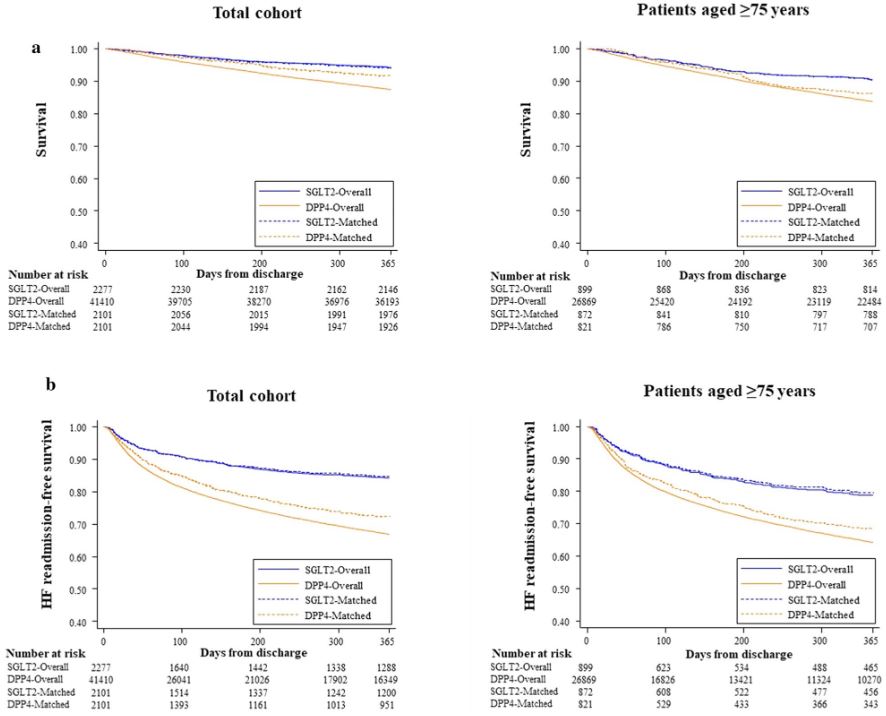
不同分组患者的生存率和心衰再住院率
在 300398 位心力衰竭患者中,216016 位(71.9%)年龄在 75 岁或以上,60999 位(20.3%)在服用抗糖尿病药物。接受 SGLT2 抑制剂治疗的患者比接受 DPP4 抑制剂治疗的患者更年轻,但病情更严重。Kaplan-Meier 分析表明,接受 SGLT2 抑制剂治疗的患者的死亡风险和 HF 再入院率较低。
在倾向匹配队列中,与使用 DPP-4 抑制剂相比,使用 SGLT2 抑制剂与较低的死亡率和心衰再入院风险相关(HR 0.70和0.52)。非常年长(≥75岁)的患者表现出相似的结果。在所有年龄组(包括≥75 岁)患有冠状动脉疾病或心房颤动并同时使用 β 受体阻滞剂、利尿剂或胰岛素的患者中也观察到了有利的疗效。
综上,使用 SGLT2 抑制剂与超老龄社会中广泛的 HF 合并 DM 患者的一年死亡率和 HF 再入院风险降低相关。
原始出处:
Nakai, M., Iwanaga, Y., Kanaoka, K. et al. Contemporary use of SGLT2 inhibitors in heart failure patients with diabetes mellitus: a comparison of DPP4 inhibitors in a nationwide electric health database of the superaged society. Cardiovasc Diabetol 21, 157 (2022). https://doi.org/10.1186/s12933-022-01586-6
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#抑制剂#
89
#BET#
52
#ASC#
48
#SGLT#
53
#DIA#
43
#2抑制剂#
63
#SGLT2抑制剂#在#糖尿病#合并#心力衰竭#患者中的当代应用情况
92
#SGLT2#
39