Clin Oral Investig:使用炭基美白牙膏刷牙是否可以美白牙齿?
2021-10-25 MedSci原创 MedSci原创
在过去的几年里,以木炭为基础的口腔护理产品已经得到了普及。近日,发表于Clin Oral Investig的一项随机试验比较了不同的炭基美白牙膏对人体釉质颜色、表面粗糙度和微硬度的影响。
在过去的几年里,以木炭为基础的口腔护理产品已经得到了普及。近日,发表于Clin Oral Investig的一项随机试验比较了不同的炭基美白牙膏对人体釉质颜色、表面粗糙度和微硬度的影响。

研究人员收集人体48颗上恒切牙,每颗牙齿制备成一个标本,随机分为4组(n=12):第1组,高露洁Total 12(CT);第2组,Body Kingdom(BK);第3组,Black is White(BW);第4组,高露洁 optic white(COW)。所有标本均经打磨抛光处理,然后接受4天的黑化处理(每天2分钟洗必泰和60分钟红茶浸泡),最后进行了为期12周的刷牙干预处理(使用上述牙膏,每天两次,每次1分钟)。使用分光光度计测量试样的颜色。使用接触式轮廓仪测量表面粗糙度(Ra),使用维氏硬度计测量微硬度(VHN)的变化。使用SEM观察每组的代表性样品。通过单因素方差分析、Welch、Fisher's、Kruskall-Wallis、Wilcoxon Sign Rank和配对t检验分析数据(P<0.05)。
结果显示,经过12周的刷牙,各组之间在颜色变化方面没有发现差异(P=0.989)。所有测试的牙膏都没有显示出临床上可接受的美白效果。除BW外,所有组别都发现表面粗糙度大幅增加(P<0.05)。CT检测发现牙齿标本微硬度增加(p=0.013),而在BK、BW和COW中没有发现变化(p>0.05)。
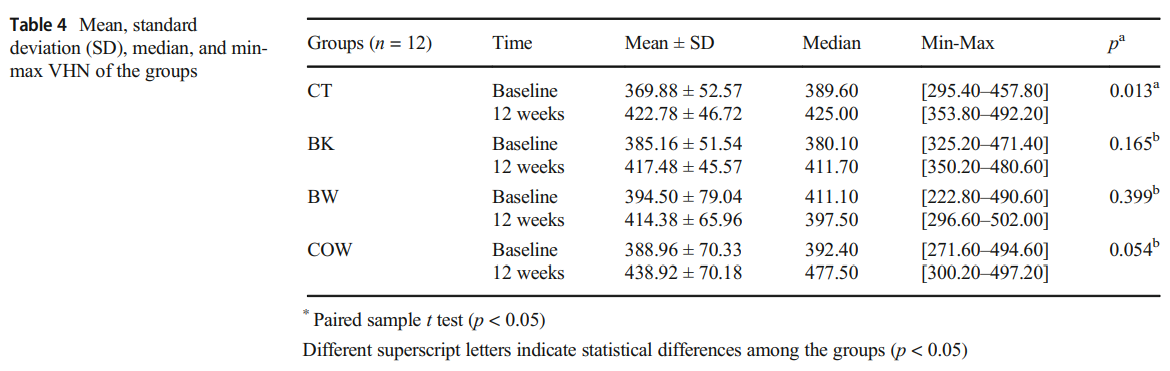
综上所述,该研究结果表明,使用炭基美白牙膏和普通氟化物牙膏刷牙12周,对牙釉质颜色的影响类似。使用炭基美白牙膏,牙齿的表面粗糙度增加(除了BW),而微硬度没有受到影响(除了CT)。
原始出处:
Uzay Koc Vural, et al., Effects of charcoal-based whitening toothpastes on human enamel in terms of color, surface roughness, and microhardness: an in vitro study. Clin Oral Investig. 2021 Oct;25(10):5977-5985. doi: 10.1007/s00784-021-03903-x.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#EST#
24
#Oral#
31
积分评论
55
#牙齿#
33